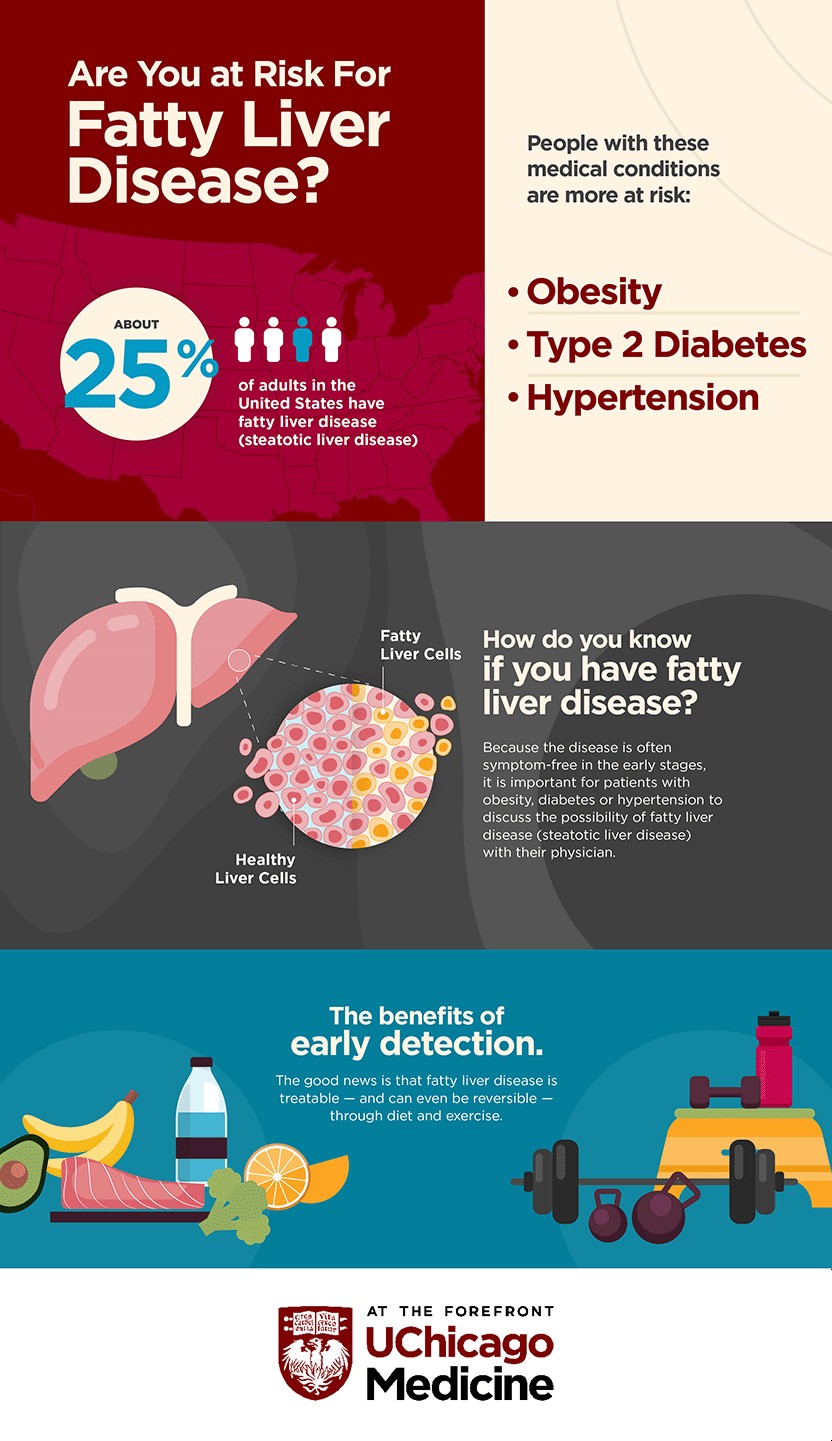
Medical professionals consistently highlight the significance of a balanced diet, yet nutritional advice isn’t always universally applicable. For individuals diagnosed with fatty liver disease, the most prevalent chronic liver ailment affecting roughly 100 million people in the United States and potentially leading to cirrhosis and liver cancer, dietary and lifestyle modifications are paramount.
As a registered dietitian and nutritionist at the University of Chicago Medicine’s Steatotic Liver Disease Clinic, I advocate for a diet abundant in healthy fats and plant-based foods, alongside up to three cups of coffee daily, to promote optimal liver health.
How to Improve Your Liver Health Through Diet
According to the American Liver Foundation, there are currently no pharmaceutical treatments available for non-alcoholic fatty liver disease. Consequently, adopting a healthy eating pattern and engaging in regular physical activity stand as the most effective strategies to prevent liver damage from developing or to reverse the condition in its early stages. Recognizing that many individuals dislike the notion of being on a restrictive “diet,” we collaborate closely with our patients to facilitate lifestyle adjustments. These encompass a nutritious diet, consistent exercise, and prioritizing sufficient, quality sleep.
What Foods Are Beneficial for Fatty Liver Disease?
You might be surprised by the recommendations. For patients managing non-alcoholic fatty liver disease, we advise consuming up to three cups of coffee each day, incorporating four tablespoons of olive oil into their daily intake, and embracing a Mediterranean diet. This dietary approach prioritizes plant-derived foods and healthy fats.
It’s often surprising for people to hear that we recommend adding foods like coffee and olive oil to their diet, rather than focusing on restrictions or eliminations.
What is an Ideal Diet Plan for a Healthy Liver?
For our patients with liver concerns, we consistently recommend the Mediterranean diet.
The Mediterranean diet aligns with typical dietitian recommendations: increased consumption of fruits and vegetables, whole grains, nuts, and legumes, lean protein sources, reduced red meat intake, and minimized consumption of sweets and added sugars.
Why is the Mediterranean Diet Recommended for Fatty Liver?
The Mediterranean diet, gaining traction in the 1990s, is more accurately described as an eating pattern than a rigid diet. It emphasizes a high intake of fruits, vegetables, whole grains, beans, nuts, legumes, olive oil, and flavorful herbs and spices. It also includes fish and seafood at least twice weekly, moderate amounts of poultry, eggs, cheese, and yogurt, while reserving sweets and red meat for occasional indulgences.
Beyond its benefits for individuals with non-alcoholic fatty liver disease, the Mediterranean diet is linked to a lower risk of heart disease. Research also indicates its effectiveness in reducing blood pressure and unfavorable LDL cholesterol levels. Furthermore, it aligns with the American Diabetes Association’s nutritional guidelines. This is particularly relevant as both heart disease and diabetes are significant risk factors strongly associated with fatty liver disease.
 Are
Are
How Dietitians Personalize Fatty Liver Disease Nutrition Plans
A crucial aspect of a dietitian’s role is to personalize nutrition plans to suit each patient’s unique needs. Every individual is different and has distinct dietary requirements and preferences.
Adopting a Mediterranean diet can be challenging due to the pervasive availability of convenience foods and less healthy options. This dietary shift requires commitment. It’s essential for patients to have dedicated time to understand the advantages of the recommended diet and to ask questions. This enables them to establish realistic and achievable goals in collaboration with a nutrition expert, increasing their likelihood of success rather than setting them up for failure.
