Is It Norovirus Or Food Poisoning? Navigating the murky waters of gastrointestinal distress can be challenging, but FOODS.EDU.VN is here to clear things up. Understanding the nuances between norovirus and food poisoning is crucial for effective management and prevention. Let’s explore the causes, symptoms, duration, and preventative measures of each condition, providing you with the knowledge to safeguard your health and well-being. This guide helps you distinguish foodborne illness and stomach bug and offer solutions to mitigate your discomfort.
1. Understanding the Culprits: What Causes Norovirus and Food Poisoning?
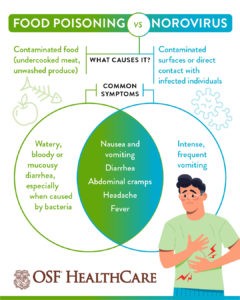
One crucial distinction between norovirus and food poisoning lies in their origins. Food poisoning stems from consuming contaminated food or beverages, often tainted with bacteria, viruses, or toxins resulting from inadequate preparation or storage. Conversely, norovirus, also known as viral gastroenteritis, is a highly contagious virus causing stomach and intestinal inflammation.
- Food Poisoning: Triggered by tainted food or drinks, harboring bacteria, viruses, or toxins due to improper handling or storage.
- Norovirus (Stomach Flu): A contagious virus inflaming the stomach and intestines, commonly spread through direct contact with infected individuals or contaminated surfaces.
Norovirus can also be transmitted via food or drink, mimicking food poisoning. It peaks during winter and results from close contact with infected people or surfaces.
1.1. Deciphering the Causes
| Cause | Description | Examples |
|---|---|---|
| Food Poisoning | Consumption of food or drink contaminated with bacteria (like Salmonella, E. coli), viruses (like Hepatitis A), or toxins (like those produced by Staphylococcus aureus). | Undercooked meat, unpasteurized dairy, contaminated produce |
| Norovirus | Viral infection spread through direct contact with infected individuals, contaminated surfaces, or consumption of contaminated food or water. Characterized by inflammation of the stomach. | Touching a contaminated doorknob, sharing utensils with an infected person, eating raw shellfish |
1.2. Research Insights
According to a study by the National Institute of Allergy and Infectious Diseases, norovirus is a leading cause of gastroenteritis globally, affecting individuals of all ages. Food poisoning, as highlighted by the Centers for Disease Control and Prevention (CDC), affects millions annually in the United States alone, emphasizing the importance of food safety practices.
 Norovirus vs Food Poisoning Causes
Norovirus vs Food Poisoning Causes
2. Spotting the Differences: Symptoms of Norovirus vs. Food Poisoning
Differentiating between norovirus and food poisoning can be challenging as their symptoms often overlap. However, subtle variations exist. Food poisoning typically manifests with nausea, vomiting, diarrhea (occasionally bloody or mucousy), and abdominal cramps. Norovirus presents with nausea, vomiting, diarrhea, abdominal cramps, low-grade fever, fatigue, and headache.
2.1. Symptom Breakdown
| Symptom | Food Poisoning | Norovirus |
|---|---|---|
| Nausea | Common | Common |
| Vomiting | Common | Common |
| Diarrhea | Common (may be bloody or contain mucus) | Common |
| Abdominal Cramps | Common | Common |
| Fever | Less common, but possible | More typical (low-grade) |
| Fatigue | Possible | Common |
| Headache | Uncommon | Common |
| Stool Appearance | May have different color or texture | Typically normal |
2.2. Expert Insights
Fever is more indicative of norovirus, although it can occur with food poisoning depending on the causative agent. Altered stool color or texture is more commonly associated with food poisoning. For accurate diagnosis and care, consult healthcare professionals.
3. Time is of the Essence: Onset and Duration
The timing and duration of symptoms can offer vital clues for distinguishing between food poisoning and norovirus. Food poisoning symptoms typically arise within one hour to three days post-consumption of contaminated food, while norovirus symptoms manifest between 12 to 72 hours after exposure. Food poisoning may last from a few hours to several days, whereas norovirus often causes a stomach flu lasting at least 24 hours, with some symptoms persisting for three days or longer.
3.1. Timeline Comparison
| Feature | Food Poisoning | Norovirus |
|---|---|---|
| Onset | 1 hour to 3 days after eating tainted food | 12 to 72 hours after exposure |
| Duration | Few hours to several days | At least 24 hours, up to 3 days or longer |
3.2. Real-World Application
If vomiting and diarrhea occur suddenly after eating, food poisoning is more likely. Contact FOODS.EDU.VN at 1946 Campus Dr, Hyde Park, NY 12538, United States, or WhatsApp: +1 845-452-9600 for additional support.
4. Contagion Factors: Spread and Prevention
Both food poisoning and norovirus can spread, but their modes of transmission differ. Norovirus is highly contagious, spreading via contact with contaminated surfaces or through direct person-to-person contact. While food poisoning is not typically considered contagious, its causative agents can spread through contaminated food and drink.
4.1. Contagion Matrix
| Condition | Contagious? | Mode of Spread |
|---|---|---|
| Food Poisoning | Sometimes | Primarily through consumption of contaminated food or drink; potential spread if the contamination source is a communicable pathogen |
| Norovirus | Yes | Highly contagious; spreads through direct contact with infected individuals, contaminated surfaces, or consumption of contaminated food or water; airborne transmission possible |
4.2. Post-Symptom Precautions
Even after recovery, norovirus can remain contagious for several days, necessitating staying home for a day or two after symptoms subside to prevent transmission.
5. Easing Discomfort: Relief Strategies for Stomach Cramps and Diarrhea
If food poisoning stems from a bacterial infection, antibiotics may be prescribed. However, for viral stomach flu or food poisoning, allowing the illness to run its course is necessary. Symptom relief strategies include hydration, bland foods, and appropriate medications.
5.1. Relief Measures
- Hydration: Opt for water in controlled increments, broth, or electrolyte solutions. A 50% Pedialyte and water mix can enhance palatability and electrolyte intake.
- Bland Foods: Embrace easy-to-digest options like bananas, rice, applesauce, and toast (BRAT diet). Shun dairy, caffeine, alcohol, nicotine, and spicy foods.
- Medications: Over-the-counter remedies like Imodium for diarrhea and Tylenol for headaches can provide relief. Doctors may prescribe anti-nausea medications as well.
5.2. Research Backing
A study published in the American Journal of Gastroenterology emphasizes the importance of oral rehydration therapy in managing diarrheal illnesses, highlighting the efficacy of electrolyte solutions in restoring fluid balance.
6. Prevention is Paramount: Guarding Against Norovirus and Food Poisoning
Washing hands with soap and water remains a cornerstone in preventing norovirus spread. When caring for someone sick, wear gloves and avoid touching your face or mouth. Regular cleaning and disinfection of high-touch surfaces like doorknobs and sinks are essential. Promptly wash soiled towels, bed sheets, and blankets in hot water. Opt for disinfectant wipes over towels and sprays for surface cleaning. Hand hygiene is equally vital in preventing food poisoning.
6.1. Prevention Checklist
- Hand Hygiene: Wash hands thoroughly with soap and water, especially before food preparation and after using the restroom.
- Surface Disinfection: Regularly clean and disinfect frequently touched surfaces.
- Food Storage: Store food at appropriate temperatures and avoid leaving it at room temperature for extended periods.
- Protective Measures: When caring for someone sick, wear gloves and practice strict hygiene.
6.2. Expert Recommendations
Ensure clean hands and disinfected food preparation areas. Store food at the correct temperature to prevent bacterial growth. When in doubt, discard questionable food items. Explore FOODS.EDU.VN for comprehensive food safety guidelines and tips.
7. When to Seek Help: Recognizing Warning Signs
For both norovirus and food poisoning, seek medical attention if vomiting or diarrhea occurs more than once per hour or lasts longer than a day. Accompanying symptoms like severe abdominal pain, blood in the stool, dry tongue, infrequent urination, or chapped lips warrant a visit to an urgent care clinic or emergency department.
7.1. Emergency Symptoms
- Severe Abdominal Pain: Intense pain that does not subside.
- Blood in Stool: Presence of blood in bowel movements.
- Dehydration Signs: Dry tongue, decreased urination, chapped lips.
- Persistent Symptoms: Vomiting or diarrhea lasting over 24 hours.
7.2. Healthcare Access
For immediate medical assistance, visit an urgent care clinic or your primary care provider’s office. In critical situations, promptly go to the emergency department.
8. Advanced Preventative Strategies
To further reduce the risk of contracting norovirus and food poisoning, consider the following advanced preventative strategies. These methods complement basic hygiene practices and enhance overall protection.
8.1. Water Purification
Ensure that drinking water is safe, especially when traveling or in areas with questionable water quality.
- Boiling: Boil water for at least 1 minute to kill viruses and bacteria.
- Filtration: Use water filters that are certified to remove viruses and bacteria.
- Chemical Treatment: Use chlorine or iodine tablets to disinfect water. Follow the manufacturer’s instructions carefully.
8.2. Safe Food Handling Practices
Adopt stringent food handling practices to minimize the risk of contamination at every stage.
- Separate Cutting Boards: Use separate cutting boards for raw meats, poultry, and seafood, and for fruits and vegetables.
- Thorough Cooking: Cook foods to their safe internal temperatures. Use a food thermometer to ensure accuracy.
- Proper Cooling: Cool leftovers quickly and store them in the refrigerator within two hours. Divide large quantities of food into smaller containers to speed up the cooling process.
- Avoid Cross-Contamination: Keep raw and cooked foods separate in the refrigerator to prevent cross-contamination.
8.3. Enhanced Hygiene Measures
Improve personal hygiene habits to minimize the spread of pathogens.
- Hand Sanitizer: Use alcohol-based hand sanitizer (at least 60% alcohol) when soap and water are not available.
- Nail Hygiene: Keep fingernails short and clean to prevent the accumulation of germs.
- Avoid Sharing Personal Items: Do not share utensils, cups, or towels with others, especially when someone is sick.
8.4. Surface Disinfection Protocols
Develop a comprehensive surface disinfection protocol, focusing on high-touch areas.
- Regular Cleaning: Clean surfaces with soap and water to remove dirt and grime before disinfecting.
- Effective Disinfectants: Use EPA-approved disinfectants that are effective against norovirus and common foodborne pathogens.
- Contact Time: Follow the disinfectant’s instructions for contact time (the amount of time the disinfectant needs to remain on the surface to kill pathogens).
- Ventilation: Ensure proper ventilation when using disinfectants to avoid inhaling harmful fumes.
8.5. Travel Precautions
Take extra precautions when traveling to areas with different sanitation standards.
- Eat at Reputable Establishments: Choose restaurants and food vendors that adhere to high hygiene standards.
- Avoid Raw Foods: Be cautious of consuming raw or undercooked foods, especially seafood and salads.
- Drink Bottled or Treated Water: Avoid drinking tap water, and use bottled or treated water for drinking, brushing teeth, and making ice.
9. Nutritional Support for Recovery
Focus on providing the body with the necessary nutrients to support recovery and restore gut health.
9.1. Probiotics
- Benefits: Probiotics help restore the balance of beneficial bacteria in the gut, which can be disrupted by norovirus or food poisoning.
- Sources: Yogurt with live and active cultures, kefir, sauerkraut, kimchi, and probiotic supplements.
- Considerations: Consult a healthcare professional before starting probiotic supplements, especially for individuals with compromised immune systems.
9.2. Prebiotics
- Benefits: Prebiotics are non-digestible fibers that feed beneficial bacteria in the gut, promoting their growth and activity.
- Sources: Garlic, onions, leeks, asparagus, bananas, oats, and apples.
- Incorporation: Include prebiotic-rich foods in the diet to support the recovery of the gut microbiome.
9.3. Gut-Healing Foods
- Bone Broth: Rich in collagen, gelatin, and amino acids, which help repair the gut lining and reduce inflammation.
- Ginger: Known for its anti-inflammatory and anti-nausea properties. Consume ginger tea or add fresh ginger to meals.
- Turmeric: Contains curcumin, a potent anti-inflammatory compound. Use turmeric in cooking or take a curcumin supplement.
- Coconut Oil: Has antimicrobial properties and can help soothe the digestive system. Use coconut oil for cooking or consume a spoonful daily.
9.4. Hydrating Fluids
- Electrolyte-Rich Drinks: Replace lost electrolytes with sports drinks, coconut water, or homemade electrolyte solutions.
- Herbal Teas: Chamomile, peppermint, and ginger teas can help soothe the digestive system and reduce nausea.
- Clear Broths: Provide essential nutrients and help maintain hydration.
9.5. Gradual Reintroduction of Foods
- Start with Bland Foods: Begin with easy-to-digest foods such as plain rice, toast, bananas, and applesauce.
- Avoid Irritants: Stay away from spicy, fatty, and highly processed foods, as well as caffeine and alcohol, until the digestive system has fully recovered.
- Monitor Tolerance: Introduce new foods gradually and monitor for any adverse reactions.
10. Environmental Control Measures
Implement measures to control the spread of pathogens in the environment, especially in shared spaces.
10.1. Air Purification
- HEPA Filters: Use air purifiers with HEPA filters to remove airborne particles, including viruses and bacteria.
- Ventilation: Ensure proper ventilation in indoor spaces to reduce the concentration of airborne pathogens.
10.2. UV-C Sanitization
- UV-C Devices: Utilize UV-C sanitization devices to disinfect surfaces and air. UV-C light can kill viruses and bacteria, but use it safely and follow the manufacturer’s instructions.
- Applications: Use UV-C devices to sanitize frequently touched surfaces, such as doorknobs, light switches, and electronic devices.
10.3. Waste Management
- Proper Disposal: Dispose of contaminated waste, such as tissues and disposable gloves, in sealed bags to prevent the spread of pathogens.
- Liners: Use liners in trash cans and empty them frequently.
- Hand Hygiene After Waste Disposal: Wash hands thoroughly with soap and water after handling waste.
10.4. Linen and Clothing Management
- Hot Water Washing: Wash linens and clothing in hot water (at least 140°F or 60°C) to kill viruses and bacteria.
- Detergent and Disinfectant: Use a detergent and a disinfectant when washing contaminated items.
- Separate Laundry: Wash contaminated items separately from other laundry.
- Dry Thoroughly: Dry items thoroughly in a hot dryer.
10.5. Monitoring and Reporting
- Track Symptoms: Keep track of symptoms and report any outbreaks to local health authorities.
- Educate Others: Share information about prevention and control measures with family, friends, and colleagues.
By integrating these advanced strategies into daily routines, individuals and communities can substantially decrease the likelihood of contracting and spreading norovirus and food poisoning, promoting a healthier and safer atmosphere for everyone.
Navigating the complexities of gastrointestinal ailments demands knowledge and proactive measures. Whether it’s food poisoning or norovirus, understanding the nuances can empower you to take control of your health. For more in-depth information, visit foods.edu.vn and explore our extensive resources. Remember, proper hygiene, safe food handling, and prompt medical attention are your greatest allies. Contact us at 1946 Campus Dr, Hyde Park, NY 12538, United States, or WhatsApp: +1 845-452-9600.