Experiencing digestive discomfort can significantly impact your daily life. Many individuals find that certain foods trigger these unpleasant symptoms. Pinpointing these trigger foods can often feel like a complex puzzle, requiring time and meticulous food journaling.
However, for a significant portion of the population, adopting a low FODMAP diet can offer a more direct path to digestive wellness.
Research has illuminated that our bodies sometimes struggle to properly digest certain types of carbohydrates known as FODMAPs. These are specific sugars, starches, and fibers present in various foods. When these FODMAPs reach the gut, they become fermented by bacteria.
By prioritizing low-Fodmap Foods and limiting high-FODMAP counterparts, individuals can effectively alleviate a range of digestive issues.
A diet low in FODMAPs has proven beneficial for many suffering from bloating, excessive gas, and Irritable Bowel Syndrome (IBS). Studies indicate that up to 75% of IBS patients experience noticeable relief shortly after starting a low FODMAP diet, with the most significant improvements often observed within the first week. This dietary approach is also valuable for those with general food intolerances, another common source of bloating, gas, and abdominal pain.
Understanding the Low FODMAP Diet
 Variety of colorful low FODMAP fruits and vegetables including bananas, oranges, carrots, and cucumbers.
Variety of colorful low FODMAP fruits and vegetables including bananas, oranges, carrots, and cucumbers.
The low FODMAP diet involves strategically limiting specific types of carbohydrates. It’s crucial to understand that this is not just another low-carb diet trend. Instead, it’s a targeted approach that focuses solely on reducing high FODMAP foods. Furthermore, the diet is highly adaptable, allowing for personalization based on individual trigger foods.
FODMAP is an acronym that stands for “Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols.” These are categories of short-chain carbohydrates that can be poorly absorbed in the small intestine.
While most people digest FODMAPs without issue, for sensitive individuals, these carbohydrates can lead to digestive distress. This is because FODMAPs are osmotic, meaning they draw water into the small intestine. They are also rapidly fermented by bacteria in the large intestine, producing gas.
This combination of increased fluid and gas production can disrupt the normal digestive process, potentially causing symptoms like gas, bloating, abdominal pain, cramping, and diarrhea.
It’s important to note that the low FODMAP diet is designed as a temporary dietary strategy. Its primary purpose is to help manage digestive symptoms while pinpointing specific FODMAPs that trigger these issues. By following a low FODMAP protocol, individuals can systematically identify their personal FODMAP sensitivities. This knowledge empowers them to tailor their long-term diet, minimizing or avoiding problematic carbohydrates while maintaining a balanced and nutritious eating pattern.
Identifying Your Personal FODMAP Food Triggers
Dietary restrictions can sometimes feel overly restrictive. However, the low FODMAP diet is fundamentally about discovery rather than deprivation. The goal is to identify your specific food triggers, as you may only be sensitive to a few FODMAP types. Once identified, you can continue to enjoy a wide variety of other foods without experiencing symptoms. Even after identifying your trigger foods, a wealth of delicious and nutritious low FODMAP options remain, spanning vegetables, fruits, proteins, nuts, grains, and even dairy alternatives.
The process of finding your FODMAP food triggers typically involves a structured three-step approach. The initial phase requires eliminating all high FODMAP foods from your diet for a defined period, usually several weeks. It’s highly recommended to collaborate with a registered dietitian or nutritionist during this process. Eliminating all high FODMAP carbohydrates and accurately identifying individual triggers while ensuring adequate nutritional intake can be challenging without professional guidance.
The three key phases are:
- Elimination: This initial phase involves strictly eliminating all high FODMAP carbohydrates for several weeks. During this period, you should monitor your symptoms closely. Many people experience symptom improvement relatively quickly, while for others, it may take a few weeks to notice a significant difference.
- Reintroduction: In the reintroduction phase, FODMAPs are systematically reintroduced, one category at a time. This step is crucial for identifying which specific FODMAPs are poorly tolerated and in what quantities. This phase helps determine your individual tolerance levels.
- Personalization: The final personalization phase involves modifying your diet based on the findings of the reintroduction phase. The aim is to expand dietary variety while carefully managing the types and amounts of FODMAP carbohydrates you consume. This tailored approach ensures long-term symptom management while promoting a nutritionally complete diet.
A dietitian or nutritionist specializing in FODMAP diets can provide invaluable support throughout this process. They can address your questions, offer low FODMAP recipes, and assist in developing healthy and satisfying low FODMAP meal and snack plans. Their expertise is key to navigating the diet effectively and achieving sustainable results.
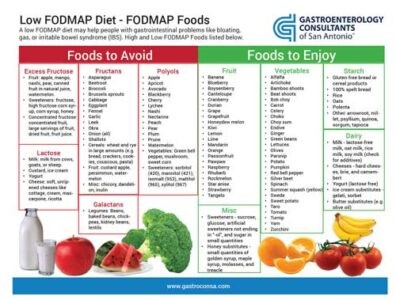
FODMAP Foods: What to Eat and What to Avoid
For those embarking on a low FODMAP diet, understanding which foods are permissible and which to avoid is paramount. Low FODMAP foods are characterized by minimal levels of fermentable carbohydrates that can trigger digestive symptoms, particularly in individuals with IBS and similar conditions. Incorporating a diverse range of low FODMAP foods is essential to ensure adequate nutrient intake while effectively managing symptoms. This section will guide you through some of the best low FODMAP food choices and highlight high FODMAP foods that should be limited or avoided.
High FODMAP Foods to Limit or Avoid:
These food categories are generally high in FODMAPs and should be restricted, especially during the elimination phase of the diet:
- Fructose: This monosaccharide is high in certain Fruits (such as apples, mangos, pears, watermelon, and dried fruits), Sweeteners like honey, high-fructose corn syrup, and agave nectar.
- Lactose: This disaccharide is the primary sugar in Dairy products including milk from cows, goats, and sheep, as well as custard, conventional yogurt, and ice cream.
- Fructans: These oligosaccharides are found in Grains like rye and wheat (in significant amounts), and certain Vegetables such as asparagus, broccoli (in large portions), cabbage, onions, and garlic.
- Galactans: These oligosaccharides are prevalent in Legumes, including beans (like baked beans), lentils, chickpeas, and soybeans.
- Polyols: These sugar alcohols are found in certain Fruits that contain pits or seeds (like apples, apricots, avocados, cherries, figs, peaches, pears, and plums), as well as artificial sweeteners like sorbitol, mannitol, xylitol, and isomalt.
Low FODMAP Foods to Enjoy:
These food categories are generally low in FODMAPs and can be included in your diet:
- Dairy Alternatives: Opt for almond milk, lactose-free milk, rice milk, coconut milk (in moderate amounts), lactose-free yogurt, and hard cheeses (like cheddar and parmesan).
- Fruits: Enjoy fruits like bananas (ripe but not overripe), blueberries, cantaloupe, grapefruit, honeydew melon, kiwi, lemon, lime, oranges, and strawberries.
- Vegetables: Choose bamboo shoots, bean sprouts, bok choy, carrots, chives, cucumbers, eggplant, ginger, lettuce, olives, parsnips, potatoes, spring onions (green parts only), and turnips.
- Protein Sources: Include beef, pork, chicken, fish, eggs, and firm tofu in your diet.
- Nuts and Seeds: (Limit portions to approximately 10-15 per serving) Almonds, macadamia nuts, peanuts, pine nuts, and walnuts are generally well-tolerated in moderation.
- Grains: Select oats, oat bran, rice bran, gluten-free pasta, quinoa, white rice, and corn flour. Note that while wheat is high FODMAP, gluten-free products are often low FODMAP, but always check labels for high FODMAP ingredients.
For personalized guidance on adopting a low FODMAP diet that meets your specific nutritional needs and preferences, consider scheduling a consultation with a registered dietitian or nutritionist specializing in gastrointestinal health. They can provide tailored advice and support.
Low FODMAP Diet vs. Gluten-Free, Vegan, or Mediterranean Diets
A low FODMAP dietary approach can be integrated with various other eating patterns.
Many gluten-free products are naturally low in FODMAPs. However, it’s important to note that not all gluten-free foods are automatically low FODMAP, so checking ingredient labels remains crucial.
Individuals following a vegan diet can successfully adhere to a low FODMAP diet by selecting plant-based protein sources that are approved on the low FODMAP list, such as tempeh and firm tofu. Careful planning is needed to ensure nutritional adequacy.
The principles of the Mediterranean diet, with its emphasis on fish, olive oil, and a wide array of vegetables, align well with low FODMAP eating. However, some Mediterranean staples, like garlic, onions, and lentils, are high in FODMAPs and would need to be modified or substituted in a low FODMAP Mediterranean diet.
While gluten-free, vegan, and Mediterranean diets are defined by the food groups they restrict or emphasize, the low FODMAP diet specifically targets types of carbohydrates known to trigger gut symptoms. Regardless of the dietary approach, careful attention to food lists and potential recipe modifications may be necessary to ensure adherence to low FODMAP principles.
FODMAP Foods List: Your Quick Guide
For a readily accessible reference, download this comprehensive FODMAP foods list in PDF format. This list provides a detailed breakdown of foods categorized as high and low FODMAP.
Frequently Asked Questions (FAQs)
What exactly does FODMAP stand for?
FODMAP is an acronym representing Fermentable Oligo-, Di-, Mono-saccharides And Polyols. These are scientific classifications for specific groups of carbohydrates recognized to trigger gastrointestinal symptoms in susceptible individuals.
Is corn considered a low FODMAP food?
Yes, corn itself is considered a low FODMAP vegetable and can be included in a low FODMAP diet. However, it’s important to differentiate corn from high-fructose corn syrup. High-fructose corn syrup is not low FODMAP due to its high concentration of fructose, a monosaccharide that is restricted on the diet.
Can I eat peanut butter on a low FODMAP diet?
Peanuts are naturally low in FODMAPs, and consequently, natural peanut butter is also generally low FODMAP. However, it’s essential to check the ingredient labels of commercial peanut butter brands. Some brands may add sweeteners or other additives that are high in FODMAPs. Typically, if any FODMAP-containing sweeteners are added, they are present in small amounts that are tolerated by most individuals on a low FODMAP diet. Choose natural peanut butter with minimal added ingredients.
Is avocado allowed on a low FODMAP diet?
Yes, avocado can be included in a low FODMAP diet, but portion control is key. A serving size of 1/8 of a whole avocado (approximately 30 grams or about two tablespoons) is considered low FODMAP. Larger portions, such as 1/4 or 1/2 of an avocado, become high in sorbitol, a polyol, and should be avoided, particularly during the elimination phase of the diet.
Tips for incorporating avocado on a low FODMAP diet:
- Carefully measure your portion size to ensure it remains at 1/8 of an avocado or less per serving.
- Spread a thin layer of avocado on low FODMAP toast or crackers.
- Add small amounts of diced avocado to salads.
- Be cautious when ordering guacamole in restaurants, as portion sizes are often larger than recommended for a low FODMAP diet.
What distinguishes a Low FODMAP diet from a Gluten-free or Dairy-free diet?
The low FODMAP diet is specifically designed to restrict particular types of carbohydrates (FODMAPs) to manage digestive symptoms, such as bloating, gas, and pain. In contrast, a gluten-free diet strictly eliminates gluten, a protein found in wheat, barley, and rye, and is primarily used for individuals with celiac disease or non-celiac gluten sensitivity. While some dairy products, like milk from cows, goats, or sheep, are high in FODMAPs (due to lactose) and are restricted on a low FODMAP diet, a dairy-free diet removes all dairy products entirely. Dairy-free diets are used to manage lactose intolerance (which is related to a FODMAP – lactose) or dairy allergies (which are protein-based and distinct from FODMAP issues). These diets have different targets and are employed for managing different digestive concerns, although there can be some overlap in food restrictions.
Could you provide some examples of low FODMAP vegetables?
Examples of low FODMAP vegetables are plentiful and include carrots, bell peppers, cucumbers, eggplant, green beans, lettuce, tomatoes, zucchini, broccoli florets (in small portions), spinach, kale, and many more. For an extensive list of low FODMAP vegetables and their appropriate serving sizes, please download the Low FODMAP Diet and Food List PDF.
What are some good Low FODMAP Snack options?
Finding convenient and satisfying low FODMAP snacks can be challenging initially. Here are some excellent low FODMAP snack ideas that are both healthy and suitable for a low FODMAP diet:
- Hard-boiled eggs: A protein-rich and portable snack.
- Rice cakes topped with peanut or almond butter (ensure no high FODMAP additives in nut butter).
- Low FODMAP fruits, such as a small banana (ripe but not overripe), a handful of grapes, or an orange. Portion control is important for fruit on a low FODMAP diet.
- Rice crackers with lactose-free cheese slices.
- Plain popcorn (air-popped or lightly oiled, without added high FODMAP flavors or seasonings).
- Gluten-free pretzels or crackers paired with tuna salad or egg salad prepared with lactose-free mayonnaise and no high FODMAP ingredients like onion.
- Roasted nuts or seeds in moderation, such as pumpkin seeds or sunflower seeds (portion control is key for nuts and seeds).
- Raw vegetable sticks like carrot sticks, cucumber slices, or bell pepper strips.
Are eggs considered low FODMAP?
Yes, eggs are inherently low in FODMAPs and are generally well-tolerated by individuals following a low FODMAP diet. Eggs are a valuable source of protein and can be prepared in numerous ways – boiled, poached, fried, scrambled, or baked. However, be mindful of ingredients commonly added to egg dishes, such as onion or garlic, which are high in FODMAPs and should be avoided or substituted with low FODMAP alternatives like chives or garlic-infused oil (garlic removed).
What is FODMAP stacking, and is it something I should be concerned about?
FODMAP stacking refers to the cumulative effect of consuming multiple low-FODMAP foods within the same meal or in close succession, where these foods contain similar types of FODMAPs. While each individual food might be low FODMAP in a typical serving, the combined effect can lead to a build-up of FODMAPs in the gut, potentially triggering symptoms. For instance, a small serving of broccoli florets may be well-tolerated, but eating it in the same meal as cauliflower and mushrooms could lead to FODMAP stacking if these vegetables contain similar FODMAP categories.
While you don’t need to become overly fixated on FODMAP stacking, it is a factor to consider if you are meticulously following a low FODMAP diet yet still experiencing persistent symptoms. Being mindful of combining multiple foods from the same FODMAP category in a single meal can be helpful for optimizing symptom management.
Are there support groups available for IBS and low FODMAP dieters?
Yes, there are numerous organizations that can assist in finding IBS support groups in your local area. Organizations like The IBS Network (in the UK) and others globally often have resources to help locate support groups and online communities. Connecting with others who are also managing IBS and following low FODMAP diets can provide valuable peer support and shared experiences. You can explore resources like IBS Support Groups to find assistance and community.
