Embark on a journey to better health with a comprehensive Diabetes Food Diet Plan, designed to manage blood sugar levels and enhance overall well-being. At FOODS.EDU.VN, we provide the resources and knowledge you need to create personalized meal plans that are both delicious and effective. Discover how to enjoy nutritious meals while keeping your diabetes in check, using expert advice and easy-to-follow guidelines. Explore various healthy eating strategies, blood sugar management techniques, and diabetic-friendly recipes to support your journey.
1. Understanding the Importance of a Diabetes Food Diet Plan
A well-structured diabetes food diet plan is crucial for managing blood sugar, weight, and overall health. It goes beyond just listing foods to eat; it’s about understanding how different foods affect your body and tailoring your meals to meet your specific needs. This comprehensive approach ensures that you get the necessary nutrients while keeping your blood sugar levels within a healthy range.
1.1. Why a Meal Plan Matters for Diabetes Management
A diabetes diet plan acts as a roadmap, guiding you on what, when, and how much to eat. This structured approach helps maintain consistent blood sugar levels, preventing drastic spikes and drops. A tailored meal plan considers your personal goals, preferences, lifestyle, and any medications you’re taking, ensuring it fits seamlessly into your daily routine.
1.2. Key Components of a Diabetes-Friendly Meal Plan
A successful diabetes meal plan should prioritize:
- Non-Starchy Vegetables: Increase your intake of nutrient-rich options like broccoli, spinach, and green beans, which have minimal impact on blood sugar.
- Reduced Added Sugars and Refined Grains: Limit foods with added sugars and refined grains, such as white bread, rice, and pasta, which can cause rapid blood sugar spikes.
- Whole Foods Focus: Emphasize whole, unprocessed foods over highly processed alternatives to maximize nutritional benefits and stabilize blood sugar levels.
By incorporating these elements, you can create a balanced and effective plan that supports your health goals.
2. The Science Behind How Food Affects Blood Sugar
Understanding how different foods impact your blood sugar is fundamental to creating an effective diabetes food diet plan. Carbohydrates are the primary nutrient that affects blood sugar levels, but the rate at which they do so varies depending on the type of food and what you eat with it.
2.1. How Carbohydrates Impact Blood Sugar Levels
Carbohydrates break down into glucose, which is then absorbed into the bloodstream, raising blood sugar levels. The glycemic index (GI) measures how quickly a food raises blood sugar. Foods with a high GI, like fruit juice, cause a rapid spike, while those with a low GI, like whole grains, are digested more slowly, leading to a gradual increase.
2.2. Balancing Carbs with Protein, Fat, and Fiber
Eating carbohydrates with protein, fat, or fiber can slow down the absorption of glucose, leading to more stable blood sugar levels. For example, pairing an apple with a handful of nuts provides fiber and fat that mitigate the impact of the fruit’s natural sugars.
A study published in the American Journal of Clinical Nutrition found that consuming protein and fat with carbohydrates significantly reduced postprandial glucose excursions in individuals with type 2 diabetes (American Journal of Clinical Nutrition, 2018).
2.3. The Importance of Regular, Balanced Meals
Regular, balanced meals are essential to avoid both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar). Eating roughly the same amount of carbohydrates at each meal helps maintain consistent blood sugar levels throughout the day. Consistency is key to managing diabetes effectively.
3. Practical Tips for Creating Your Diabetes Food Diet Plan
Creating a diabetes food diet plan doesn’t have to be overwhelming. By using simple techniques like carb counting and the plate method, you can create a meal plan that is both manageable and effective.
3.1. Carb Counting: A Detailed Guide
Carb counting involves tracking and limiting the number of carbohydrates you consume at each meal. This method helps you match your insulin dosage (if applicable) to your carbohydrate intake, providing better blood sugar control.
3.1.1. Determining Your Carb Goals
Work with your doctor or a registered dietitian to determine the appropriate amount of carbohydrates you should aim for each day. This number will depend on your individual needs, activity level, and any medications you are taking.
3.1.2. Using Carbohydrate Lists and Food Labels
Refer to comprehensive lists of common foods and their carbohydrate content. Pay close attention to serving sizes, as carbohydrate counts are based on specific portions. Food labels are also an invaluable resource, providing detailed information about carbohydrate content per serving.
For example, a slice of whole wheat bread typically contains around 15 grams of carbohydrates, while a cup of cooked rice can have about 45 grams. Being aware of these values helps you make informed choices and stay within your carb targets.
3.1.3. Tools and Apps for Carb Tracking
Numerous apps and online tools are available to help you track your carbohydrate intake. Apps like MyFitnessPal, Carb Manager, and Figwee Calorie Counter allow you to log your meals and calculate the carbohydrate content automatically. These tools can simplify the carb counting process and provide valuable insights into your eating habits.
3.2. The Plate Method: A Simple Visual Guide
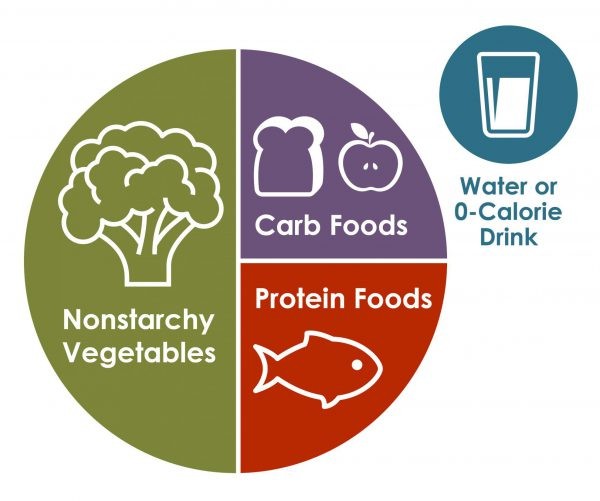
The plate method is a straightforward visual tool that helps you balance the proportions of different food groups in your meals. It encourages a balanced intake of vegetables, lean protein, and carbohydrates.
3.2.1. How to Divide Your Plate
Start with a 9-inch dinner plate (about the length of a standard business envelope). Divide the plate as follows:
- Half of the Plate: Fill this portion with non-starchy vegetables such as salad, green beans, broccoli, or spinach.
- One Quarter of the Plate: Fill this portion with lean protein sources like chicken, turkey, fish, beans, tofu, or eggs.
- One Quarter of the Plate: Fill this portion with carbohydrate-rich foods such as grains, starchy vegetables (potatoes, peas, corn), rice, pasta, beans, fruit, or yogurt.
3.2.2. Choosing the Right Foods for Each Section
- Non-Starchy Vegetables: These are low in carbohydrates and high in fiber, making them an excellent choice for filling up your plate. Examples include leafy greens, cucumbers, bell peppers, and cauliflower.
- Lean Protein: Choose lean protein sources to support muscle health and satiety. Examples include grilled chicken breast, baked fish, tofu, and lentils.
- Carbohydrate-Rich Foods: Opt for whole grains and complex carbohydrates over refined grains and simple sugars. Examples include brown rice, quinoa, whole wheat bread, and sweet potatoes.
3.2.3. Adding a Beverage
Complete your meal with water or a low-calorie beverage like unsweetened iced tea. Avoid sugary drinks like soda and juice, which can cause rapid blood sugar spikes.
The plate method is a visual guide to help you balance your meals with vegetables, protein, and carbohydrates.
3.3. Portion Control: Understanding Serving Sizes
Understanding portion sizes is crucial for managing both weight and blood sugar. A portion is the amount of food you choose to eat at one time, while a serving is a specific, measured amount of food. It’s easy to unintentionally consume more calories and carbohydrates if you’re not mindful of portion sizes.
3.3.1. Portion vs. Serving Size
Be aware that portion sizes at restaurants and in packaged foods often exceed recommended serving sizes. This can lead to overeating and difficulty in managing blood sugar levels.
3.3.2. Tips for Controlling Portion Sizes
- Eating Out: When dining out, ask for half of your meal to be wrapped up to go before you start eating. This helps prevent overconsumption and allows you to enjoy the leftovers later.
- At Home: Measure out snacks instead of eating directly from the bag or box. This prevents mindless snacking and helps you stay within your portion limits.
- During Meals: Reduce the temptation to go back for seconds by keeping serving bowls out of reach. This makes you more conscious of your food intake.
3.3.3. The Handy Guide to Portion Sizes
Use the following “handy” guide to estimate portion sizes on the go:
| Food | Portion Size | Hand Reference |
|---|---|---|
| Meat, Fish, or Poultry (3 ounces) | Palm of hand (no fingers) | Approximate size of your palm |
| Cheese or Meat (1 ounce) | Thumb (tip to base) | Size of your thumb from tip to base |
| Fruit or Cooked Veggies (1 cup) | Fist | Size of your closed fist |
| Nuts or Pretzels (1–2 ounces) | Cupped hand | What fits in your cupped hand |
| Butter, Oil, or Sugar (1 Tablespoon) | Thumb tip (tip to 1st joint) | Size of your thumb tip |
| Butter, Oil, or Sugar (1 Teaspoon) | Fingertip (tip to 1st joint) | Size of your fingertip |
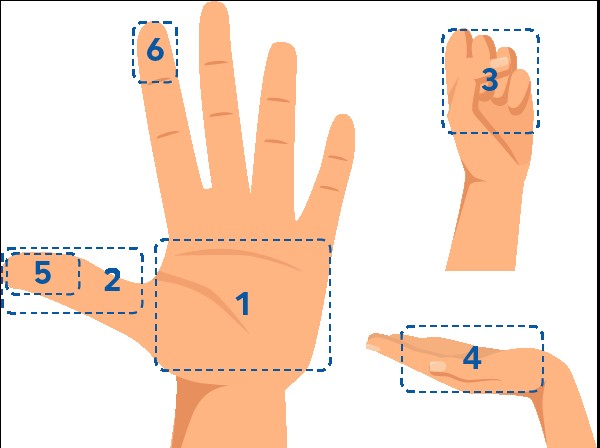
Use this handy guide to estimate portion sizes when you’re on the go.
4. Delicious and Healthy Recipes for Your Diabetes Food Diet Plan
Creating a diabetes food diet plan doesn’t mean sacrificing flavor. Numerous delicious and healthy recipes can help you manage your blood sugar while enjoying your meals.
4.1. Sample Meal Plan
Here’s a sample one-day meal plan that includes a variety of nutritious and diabetes-friendly options:
- Breakfast (45-60g carbs): Oatmeal with berries and nuts, a sprinkle of cinnamon.
- Lunch (45-60g carbs): Large salad with grilled chicken, avocado, and a light vinaigrette dressing.
- Dinner (45-60g carbs): Baked salmon with roasted vegetables (broccoli, carrots, and bell peppers)
- Snacks (15-30g carbs): A small apple with almond butter, or a handful of mixed nuts.
4.2. Breakfast Recipes
Start your day with these nutritious and delicious breakfast options:
- Oatmeal with Berries and Nuts: A classic choice that is high in fiber and antioxidants.
- Greek Yogurt with Fruit and Seeds: A protein-packed option that keeps you full and energized.
- Whole-Wheat Toast with Avocado and Egg: A balanced meal with healthy fats, protein, and complex carbohydrates.
4.3. Lunch Recipes
Enjoy these satisfying and diabetes-friendly lunch ideas:
- Quinoa Salad with Roasted Vegetables and Chickpeas: A nutrient-rich salad with plant-based protein and fiber.
- Turkey and Avocado Wrap: A convenient and balanced meal that is easy to take on the go.
- Lentil Soup: A hearty and filling soup that is low in fat and high in fiber.
4.4. Dinner Recipes
End your day with these flavorful and healthy dinner options:
- Baked Salmon with Roasted Vegetables: A protein-rich meal with healthy fats and plenty of vitamins and minerals.
- Chicken Stir-Fry with Brown Rice: A quick and easy meal with lean protein and complex carbohydrates.
- Black Bean Burgers on Whole-Wheat Buns: A vegetarian option that is high in protein and fiber.
5. Navigating Challenges and Maintaining Consistency
Even with a well-planned diabetes food diet plan, you may encounter challenges. It’s important to develop strategies to overcome these obstacles and maintain consistency.
5.1. Common Pitfalls and How to Avoid Them
- Emotional Eating: Develop strategies to manage stress and emotional triggers that lead to unhealthy eating habits.
- Eating Out: Plan ahead by checking menus online and making informed choices.
- Holiday and Special Occasions: Balance indulgence with healthy choices and practice portion control.
5.2. Staying Motivated and Avoiding Burnout
- Set Realistic Goals: Start with small, achievable changes and gradually work towards larger goals.
- Track Your Progress: Use a food diary or app to monitor your food intake and progress towards your goals.
- Reward Yourself: Celebrate your successes with non-food rewards, such as a relaxing activity or a new book.
5.3. Building a Support System
- Family and Friends: Enlist the support of your loved ones to help you stay on track.
- Diabetes Support Groups: Connect with others who have diabetes to share experiences and tips.
- Healthcare Professionals: Work with your doctor, dietitian, or diabetes educator to develop a personalized plan and address any concerns.
6. The Role of Exercise in Your Diabetes Management Plan
While diet is crucial, incorporating regular physical activity into your routine is essential for managing diabetes. Exercise helps improve insulin sensitivity, lower blood sugar levels, and promote overall health.
6.1. Benefits of Regular Physical Activity
- Improved Blood Sugar Control: Exercise helps your body use insulin more effectively, leading to better blood sugar control.
- Weight Management: Physical activity helps you burn calories and maintain a healthy weight.
- Reduced Risk of Complications: Regular exercise can reduce your risk of developing diabetes-related complications, such as heart disease and nerve damage.
6.2. Types of Exercise to Consider
- Aerobic Exercise: Activities like walking, jogging, swimming, and cycling can improve your cardiovascular health and lower blood sugar levels.
- Strength Training: Lifting weights or using resistance bands can help build muscle mass, which improves insulin sensitivity.
- Flexibility Exercises: Stretching and yoga can improve your range of motion and reduce your risk of injury.
6.3. Tips for Incorporating Exercise into Your Daily Routine
- Start Slowly: Begin with small amounts of exercise and gradually increase the intensity and duration.
- Find Activities You Enjoy: Choose activities that you find fun and engaging to increase the likelihood that you’ll stick with them.
- Make It a Habit: Schedule exercise into your daily routine and treat it like any other important appointment.
7. Monitoring Your Blood Sugar Levels
Regularly monitoring your blood sugar levels is crucial for understanding how your diabetes food diet plan and exercise routine are affecting your health. This information helps you make informed decisions about your diet, medication, and activity levels.
7.1. Understanding Blood Sugar Testing
- Frequency of Testing: Work with your doctor to determine how often you should test your blood sugar.
- Types of Blood Glucose Meters: Choose a meter that is easy to use and meets your needs.
- Proper Testing Technique: Follow the instructions provided with your meter to ensure accurate results.
7.2. Interpreting Your Results
- Target Blood Sugar Ranges: Know your target blood sugar ranges and understand what they mean.
- Recognizing Patterns: Look for patterns in your blood sugar levels to identify how different foods and activities affect your body.
- Adjusting Your Plan: Use your blood sugar readings to make adjustments to your diet, exercise routine, or medication as needed.
7.3. Continuous Glucose Monitoring (CGM)
- Benefits of CGM: Continuous glucose monitors provide real-time blood sugar readings and track your levels over time, providing valuable insights into your glucose patterns.
- How CGM Works: A small sensor is inserted under your skin and measures glucose levels in your interstitial fluid.
- Using CGM Data: Use the data from your CGM to identify trends, make adjustments to your diet and exercise routine, and improve your overall diabetes management.
8. Seeking Professional Support and Education
While this guide provides valuable information, working with healthcare professionals is essential for creating a diabetes food diet plan that meets your unique needs.
8.1. The Role of a Registered Dietitian
A registered dietitian specializing in diabetes can help you:
- Develop a Personalized Meal Plan: Create a meal plan that takes into account your individual needs, preferences, and health goals.
- Learn Carb Counting Techniques: Master the art of carb counting to better manage your blood sugar levels.
- Make Healthy Food Choices: Understand how to choose the right foods for your diabetes management plan.
8.2. Diabetes Self-Management Education and Support (DSMES)
DSMES programs provide comprehensive education and support to help you:
- Understand Diabetes: Learn about the disease, its complications, and how to manage it effectively.
- Develop Problem-Solving Skills: Learn how to identify and address challenges that may arise in your diabetes management journey.
- Improve Your Quality of Life: Enhance your overall well-being and live a full and active life with diabetes.
8.3. Finding Resources and Support
- American Diabetes Association (ADA): The ADA offers a wealth of information and resources for people with diabetes, including meal plans, recipes, and support groups.
- Centers for Disease Control and Prevention (CDC): The CDC provides information on diabetes prevention, management, and research.
- Local Hospitals and Clinics: Many hospitals and clinics offer diabetes education programs and support services.
9. Latest Trends and Research in Diabetes Nutrition
Staying informed about the latest trends and research in diabetes nutrition can help you optimize your diabetes food diet plan and improve your health outcomes.
9.1. Emerging Diets and Nutritional Strategies
- Low-Carbohydrate Diets: Some studies suggest that low-carbohydrate diets can be effective for managing blood sugar levels and promoting weight loss in people with diabetes.
- Mediterranean Diet: The Mediterranean diet, which is rich in fruits, vegetables, whole grains, and healthy fats, has been shown to improve blood sugar control and reduce the risk of heart disease in people with diabetes.
- Plant-Based Diets: Plant-based diets, which emphasize whole, unprocessed plant foods, can be beneficial for managing diabetes and promoting overall health.
9.2. The Impact of Gut Health on Diabetes
Research suggests that the gut microbiome, the community of microorganisms living in your digestive tract, plays a role in diabetes development and management.
- Probiotics: Consuming probiotics, which are beneficial bacteria, may improve blood sugar control and insulin sensitivity.
- Prebiotics: Eating prebiotics, which are foods that feed beneficial bacteria, can promote a healthy gut microbiome.
- Fiber: A high-fiber diet can promote the growth of beneficial bacteria and improve blood sugar control.
9.3. Personalized Nutrition for Diabetes
Advances in technology and research are paving the way for personalized nutrition plans that take into account your unique genetic makeup, microbiome, and lifestyle factors.
- Genetic Testing: Genetic testing can identify specific genes that may affect your risk of developing diabetes and your response to different diets.
- Microbiome Analysis: Analyzing your gut microbiome can provide insights into your digestive health and help you tailor your diet to promote a healthy gut.
- Wearable Technology: Wearable devices can track your activity levels, sleep patterns, and blood sugar levels, providing valuable data for creating a personalized diabetes management plan.
| Trend | Description | Benefits | Considerations |
|---|---|---|---|
| Low-Carb Diets | Focuses on reducing carbohydrate intake to manage blood sugar levels. | Effective for blood sugar control and weight loss. | Requires careful monitoring and may not be suitable for everyone. |
| Mediterranean Diet | Emphasizes fruits, vegetables, whole grains, and healthy fats. | Improves blood sugar control, reduces heart disease risk, and supports overall health. | Focuses on whole foods and balanced nutrition. |
| Plant-Based Diets | Primarily consists of plant-based foods, such as fruits, vegetables, legumes, and whole grains. | Can improve blood sugar control, promote weight loss, and reduce the risk of chronic diseases. | Requires careful planning to ensure adequate nutrient intake, especially vitamin B12 and iron. |
| Gut Health Focus | Emphasizes the importance of a healthy gut microbiome for overall health and diabetes management. | Can improve blood sugar control, enhance insulin sensitivity, and support immune function. | Involves consuming probiotics, prebiotics, and fiber-rich foods. |
| Personalized Nutrition | Tailors dietary recommendations based on individual genetic makeup, microbiome, and lifestyle factors. | Optimizes health outcomes by addressing individual needs and responses to different diets. | Requires access to genetic testing, microbiome analysis, and wearable technology. |
| High-Fiber Diet | Involves increasing fiber intake from sources like whole grains, legumes, fruits, and vegetables. | Promotes stable blood sugar levels, improves digestion, and helps manage weight. | Gradual increase to avoid digestive discomfort; stay hydrated. |
| Mindful Eating Practices | Focuses on being fully present and aware during meal times to improve food choices and portion control. | Enhanced awareness of hunger and fullness cues, better portion control, and reduced emotional eating. | Requires practice and patience; involves reducing distractions during meals. |
| Intermittent Fasting | Involves cycling between periods of eating and voluntary fasting on a regular schedule. | May improve insulin sensitivity, support weight loss, and enhance cellular repair. | Requires careful planning and monitoring; not suitable for everyone, especially those on certain medications or with specific health conditions. |
| Glycemic Index (GI) and Glycemic Load (GL) | Focuses on choosing foods with lower GI and GL to manage blood sugar levels. | Helps prevent rapid spikes in blood sugar levels after meals. | Involves understanding GI and GL values of various foods. |
| Continuous Glucose Monitoring (CGM) | Utilizes devices to track glucose levels in real-time, providing valuable insights into glucose patterns and responses to food and exercise. | Provides continuous data to make informed decisions about diet and lifestyle; enhances diabetes management. | Requires wearing a device and regular calibration. |
10. FAQs About Diabetes Food Diet Plans
Here are some frequently asked questions about diabetes food diet plans:
- What is a diabetes food diet plan?
- A structured eating plan designed to help manage blood sugar levels by controlling carbohydrate intake and promoting balanced nutrition.
- Why is a meal plan important for diabetes?
- It helps maintain consistent blood sugar levels, preventing spikes and drops, and supports overall health.
- What foods should I include in my diabetes diet?
- Non-starchy vegetables, lean proteins, whole grains, and healthy fats.
- Are there foods I should avoid if I have diabetes?
- Sugary drinks, processed foods, refined grains, and foods high in saturated and trans fats.
- How do I count carbohydrates?
- Use food labels, carbohydrate lists, and tracking apps to monitor your carb intake at each meal.
- What is the plate method?
- A visual guide to balance your meals with half the plate filled with non-starchy vegetables, one quarter with lean protein, and one quarter with carbohydrate-rich foods.
- How often should I monitor my blood sugar levels?
- Work with your doctor to determine the appropriate frequency based on your individual needs.
- Can exercise help manage my diabetes?
- Yes, regular physical activity improves insulin sensitivity and helps lower blood sugar levels.
- Should I see a registered dietitian?
- Yes, a dietitian can help you develop a personalized meal plan and learn effective diabetes management techniques.
- Where can I find more information and support?
- Organizations like the American Diabetes Association and the Centers for Disease Control and Prevention offer valuable resources and support.
Creating and adhering to a diabetes food diet plan is a powerful step towards managing your health and improving your quality of life. Remember, consistency, informed choices, and professional support are key to achieving your goals.
Ready to take control of your diabetes with a personalized meal plan? Visit foods.edu.vn for more delicious recipes, expert tips, and comprehensive guides to healthy eating. Our resources will empower you to create a diabetes food diet plan that fits your lifestyle and helps you thrive. Contact us today at 1946 Campus Dr, Hyde Park, NY 12538, United States, or call us on Whatsapp at +1 845-452-9600.