How Does Food Turn Into Feces? The process of how food becomes feces involves chewing, digestion, absorption, and elimination, as explained comprehensively by FOODS.EDU.VN. Understanding this process can help you make informed dietary choices and appreciate the complexity of the human body. Let’s explore the journey from your plate to the toilet, examining the key stages and organs involved, offering nutritional insights and digestive health tips.
1. What Happens When You Eat?
Eating isn’t just about enjoying flavors; it’s the start of a complex process that provides your body with the nutrients it needs. So, what exactly happens when you take that first bite?
1.1. The Initial Breakdown: Chewing and Saliva
Chewing, or mastication, is the first step in digestion. It physically breaks down food into smaller particles, making it easier to swallow and digest. Saliva, produced by the salivary glands, moistens the food and contains enzymes like amylase, which starts the chemical digestion of carbohydrates.
- Why it’s important: Proper chewing eases the burden on your stomach and intestines.
- Nutritional note: Some foods require more chewing, which can increase satiety and help with weight management.
1.2. Swallowing: The Epiglottis and Esophagus
Once you’ve chewed your food into a manageable bolus (a soft, rounded mass), it’s time to swallow. The epiglottis, a small flap of cartilage in your throat, plays a crucial role by preventing food from entering your trachea (windpipe) and directing it into the esophagus.
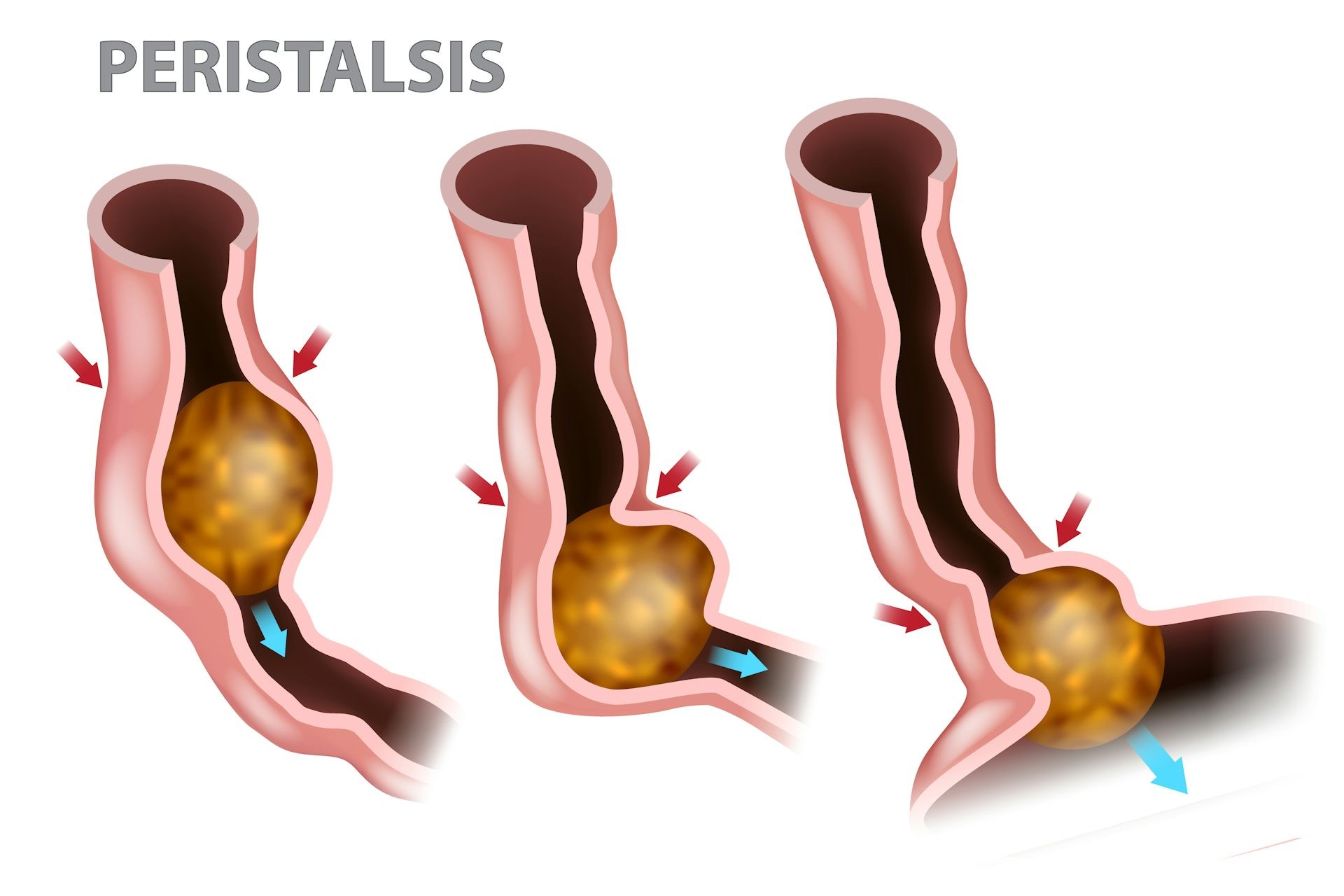
The esophagus is a muscular tube that connects your throat to your stomach. It propels the bolus downward through a series of rhythmic contractions called peristalsis. This process ensures that food moves efficiently toward your stomach, regardless of whether you’re standing up, sitting down, or even upside down.
- How peristalsis works: Muscles in the esophageal walls contract and relax in a coordinated manner, creating a wave-like motion that pushes the food bolus along.
- Fun fact: Peristalsis is so effective that it can even move food against gravity.
1.3. Stomach Action: Mixing and Grinding
The stomach is a J-shaped organ that acts as a temporary storage tank and a powerful mixing bowl. When the food bolus enters the stomach, it triggers the release of gastric juices containing hydrochloric acid and enzymes like pepsin.
Hydrochloric acid helps to denature proteins, breaking them down into smaller peptides. Pepsin, in turn, breaks down these peptides into amino acids, the building blocks of proteins. The stomach’s muscular walls churn and mix the food bolus with these gastric juices, creating a semi-liquid mixture called chyme.
- Role of gastric juices: Gastric juices contain hydrochloric acid, which helps to denature proteins and kill bacteria, and enzymes like pepsin, which break down proteins into amino acids.
- Importance of stomach acidity: The acidic environment of the stomach is essential for activating pepsin and protecting against harmful bacteria.
- Enzyme activity: Pepsin breaks down proteins, while other enzymes such as gastric lipase begin the digestion of fats.
1.4. Emptying the Stomach: Pyloric Sphincter
The pyloric sphincter, located at the lower end of the stomach, controls the rate at which chyme enters the small intestine. It gradually releases small amounts of chyme into the duodenum, the first part of the small intestine, allowing for efficient digestion and absorption.
- Regulation of chyme release: The pyloric sphincter ensures that chyme enters the small intestine at a controlled rate, preventing it from being overwhelmed.
- Factors affecting emptying rate: The rate at which the stomach empties depends on factors such as the composition of the meal (e.g., high-fat meals take longer to empty) and individual differences in digestive function.
2. What Role Does the Small Intestine Play?
The small intestine is the primary site for nutrient absorption. It’s here that most of the vitamins, minerals, proteins, carbohydrates, and fats from your food are absorbed into your bloodstream.
2.1. The Duodenum: Initial Digestion and Bile
The duodenum, the first section of the small intestine, is where chyme mixes with digestive juices from the pancreas and bile from the liver. These fluids neutralize the acidic chyme and further break down nutrients.
- Pancreatic juices: Contain enzymes such as amylase (to digest carbohydrates), lipase (to digest fats), and protease (to digest proteins).
- Bile: Emulsifies fats, breaking them into smaller droplets that are easier to digest and absorb.
- Neutralization: The alkaline nature of pancreatic juices helps to neutralize the acidic chyme, protecting the intestinal lining from damage.
2.2. The Jejunum and Ileum: Nutrient Absorption
The jejunum and ileum are the middle and final sections of the small intestine, respectively. These sections are lined with villi and microvilli, tiny finger-like projections that increase the surface area for absorption.
- Villi and microvilli: These structures greatly increase the surface area of the small intestine, allowing for maximum nutrient absorption.
- Absorption mechanisms: Nutrients are absorbed through various mechanisms, including active transport, passive diffusion, and facilitated diffusion.
- Specific nutrient absorption: Different nutrients are absorbed in different regions of the small intestine. For example, iron is primarily absorbed in the duodenum, while vitamin B12 is absorbed in the ileum.
2.3. Key Nutrients Absorbed
The small intestine absorbs a wide range of nutrients, including:
- Carbohydrates: Broken down into simple sugars like glucose.
- Proteins: Broken down into amino acids.
- Fats: Broken down into fatty acids and glycerol.
- Vitamins: Essential for various bodily functions.
- Minerals: Important for bone health, nerve function, and more.
Here’s a summary of the nutrients absorbed and their importance:
| Nutrient | Breakdown Product | Importance |
|---|---|---|
| Carbohydrates | Glucose | Primary source of energy for the body, fuels brain function, and supports physical activity. |
| Proteins | Amino Acids | Building blocks for tissues, enzymes, and hormones, essential for growth, repair, and maintenance of body structures. |
| Fats | Fatty Acids | Provide energy, support cell growth, protect organs, help absorb fat-soluble vitamins, and are crucial for hormone production. |
| Vitamins | Various | Essential for numerous bodily functions, including immune function, bone health, energy production, and protection against cell damage. |
| Minerals | Various | Important for bone health, nerve function, muscle contraction, fluid balance, and various enzymatic reactions. |
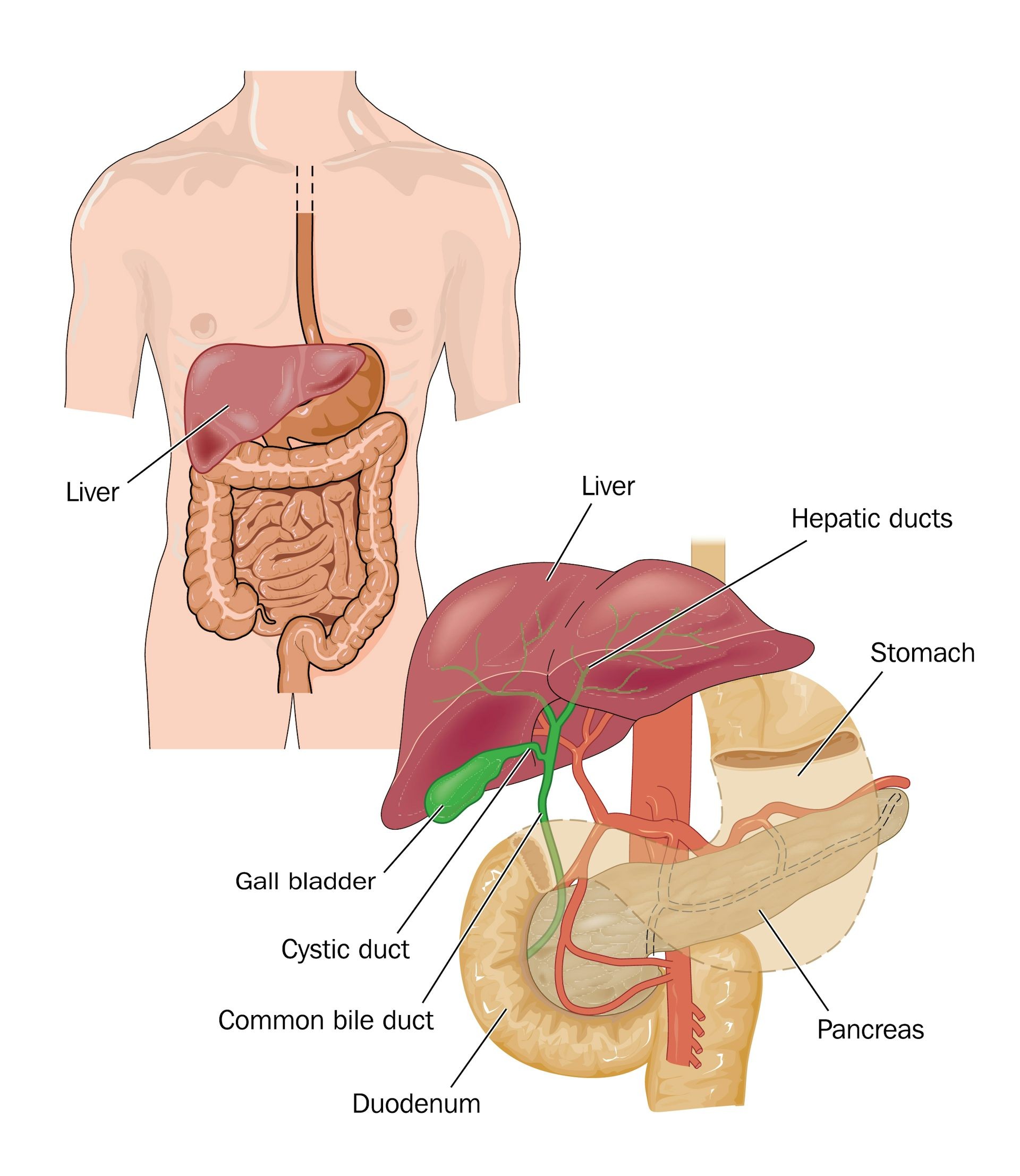
2.4. What is the Role of the Liver and Pancreas?
The liver and pancreas are vital accessory organs that play crucial roles in digestion.
- Liver: Produces bile, which emulsifies fats, breaking them into smaller droplets that are easier to digest and absorb.
- Pancreas: Produces digestive enzymes that break down carbohydrates, proteins, and fats in the small intestine. It also produces bicarbonate, which neutralizes the acidic chyme entering the small intestine from the stomach.
- Hormonal regulation: Both organs also produce hormones that regulate digestion and blood sugar levels.
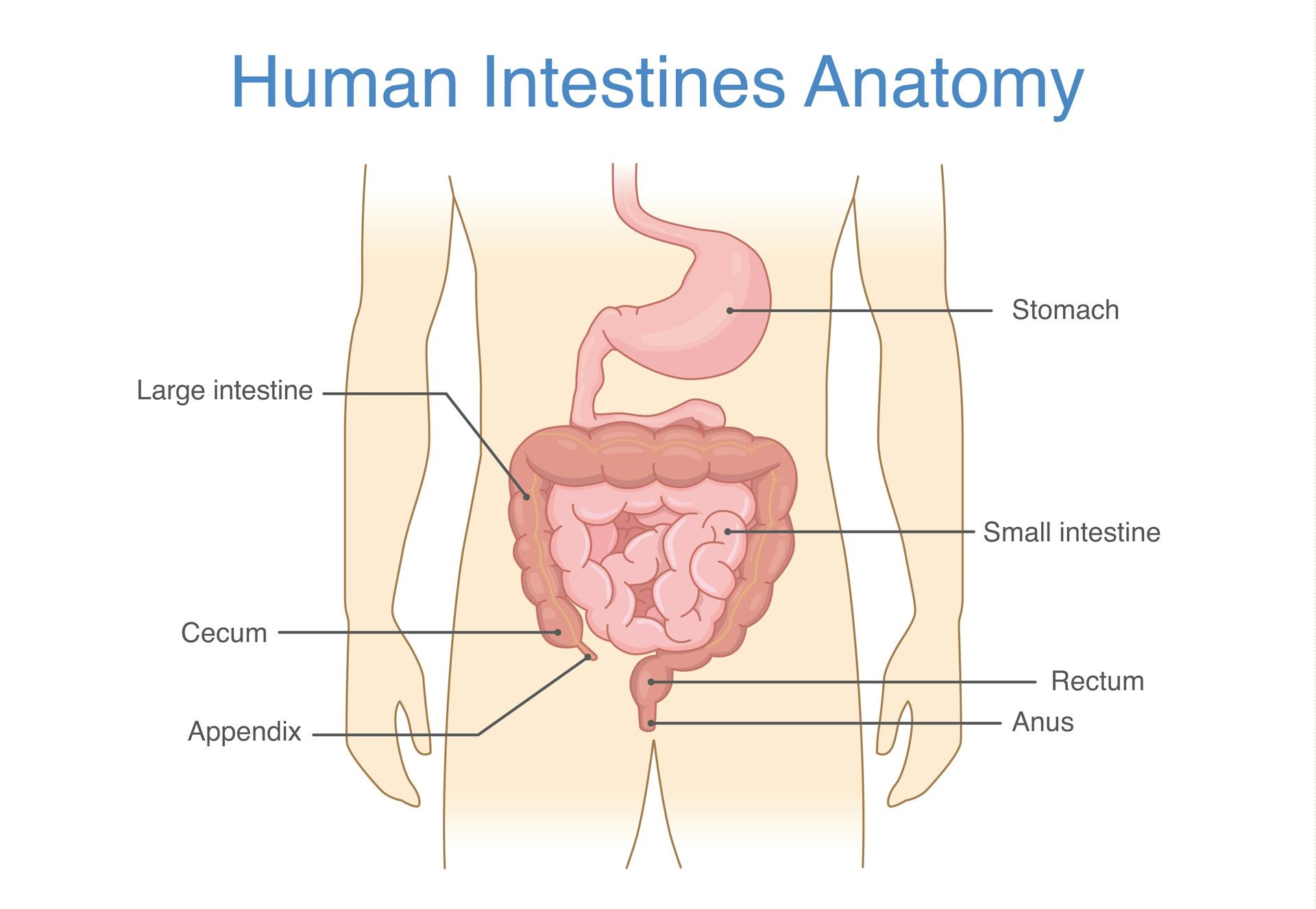
3. What Happens in the Large Intestine?
The large intestine, also known as the colon, receives the undigested food and waste products from the small intestine. Its primary functions include absorbing water and electrolytes, forming feces, and housing beneficial bacteria.
3.1. Water Absorption and Electrolyte Balance
As the waste material moves through the large intestine, water and electrolytes (such as sodium and potassium) are absorbed back into the bloodstream. This process helps to concentrate the waste material and form solid feces.
- Efficiency of water absorption: The large intestine can absorb a significant amount of water, helping to prevent dehydration.
- Electrolyte regulation: The absorption and secretion of electrolytes in the large intestine help to maintain electrolyte balance in the body.
- Consequences of impaired absorption: If the large intestine is unable to absorb water properly (e.g., due to infection or inflammation), it can result in diarrhea.
3.2. The Gut Microbiome: Beneficial Bacteria
The large intestine is home to trillions of bacteria, collectively known as the gut microbiome. These bacteria play a vital role in digestion, immunity, and overall health.
- Functions of gut bacteria: Aid in the fermentation of undigested carbohydrates, synthesize vitamins (such as vitamin K and B vitamins), and protect against harmful pathogens.
- Impact on health: A healthy gut microbiome is associated with improved digestion, a stronger immune system, and a reduced risk of chronic diseases.
- Factors affecting gut health: Diet, antibiotics, stress, and other factors can influence the composition and function of the gut microbiome.
3.3. Formation of Feces: Waste Products
The remaining waste material, consisting of undigested food, bacteria, and other waste products, is gradually formed into feces. The feces are stored in the rectum, the final section of the large intestine, until they are eliminated from the body during a bowel movement.
- Composition of feces: Feces are composed of water, undigested food, bacteria, dead cells, and other waste products.
- Factors affecting fecal consistency: Factors such as diet, hydration, and gut motility can influence the consistency of feces.
- Importance of regular bowel movements: Regular bowel movements are essential for removing waste products from the body and preventing constipation.
3.4. Storage and Elimination: The Rectum and Anus
The rectum stores feces until a bowel movement is triggered. The anus, the opening through which feces are eliminated, is controlled by two sphincters: the internal anal sphincter (involuntary) and the external anal sphincter (voluntary).
- Mechanism of defecation: When the rectum is full, it triggers the urge to defecate. The internal anal sphincter relaxes automatically, while the external anal sphincter can be consciously controlled to delay or initiate a bowel movement.
- Factors affecting bowel habits: Factors such as diet, hydration, physical activity, and stress can influence bowel habits.
- Importance of proper hygiene: Proper hygiene, including washing hands after using the toilet, is essential for preventing the spread of infection.
4. Understanding Stool: What Your Feces Tell You
Your stool can offer valuable insights into your digestive health. Observing the color, consistency, and frequency of your bowel movements can help you identify potential problems.
4.1. Bristol Stool Chart: Types of Stool
The Bristol Stool Chart is a useful tool for classifying the form of human feces into seven categories. It’s used in both clinical and experimental settings.
| Type | Appearance | Description |
|---|---|---|
| 1 | Separate hard lumps, like nuts (hard to pass) | Indicates severe constipation; likely to cause pain and may require medical attention. |
| 2 | Sausage-shaped, but lumpy | Suggests constipation; often requires more effort to pass and may be uncomfortable. |
| 3 | Like a sausage but with cracks on the surface | Generally considered normal, but can indicate mild constipation if infrequent. |
| 4 | Like a sausage or snake, smooth and soft | Considered ideal; indicates healthy bowel movements and efficient digestion. |
| 5 | Soft blobs with clear-cut edges (passed easily) | Indicates a lack of fiber in the diet; bowel movements are frequent and less formed. |
| 6 | Fluffy pieces with ragged edges, a mushy stool | Suggests mild diarrhea; may be caused by stress, diet changes, or mild infections. |
| 7 | Watery, no solid pieces (entirely liquid) | Indicates severe diarrhea; often caused by infections, food poisoning, or inflammatory bowel diseases; seek medical advice. |
4.2. Color Variations: What They Mean
The color of your stool can vary depending on your diet, medications, and overall health.
- Brown: Normal and healthy.
- Green: May indicate that food is moving through the large intestine too quickly, or that you’ve eaten a lot of green leafy vegetables.
- Yellow: Could indicate a problem with bile production or absorption.
- Black: May be caused by iron supplements or bleeding in the upper digestive tract.
- Red: Could indicate bleeding in the lower digestive tract.
- White or clay-colored: May indicate a blockage in the bile ducts.
4.3. Consistency and Frequency: What’s Normal?
The consistency and frequency of bowel movements vary from person to person.
- Consistency: Stool should be soft and formed, but not too hard or too loose.
- Frequency: Normal bowel movement frequency ranges from three times a day to three times a week.
- Changes to watch for: Sudden changes in consistency or frequency, especially if accompanied by other symptoms, should be evaluated by a healthcare professional.
5. Common Digestive Issues and Solutions
Digestive issues are common, but understanding them can help you take proactive steps to improve your gut health.
5.1. Constipation: Causes and Relief
Constipation is characterized by infrequent bowel movements and hard, difficult-to-pass stools.
- Common causes: Low fiber intake, dehydration, lack of physical activity, certain medications, and underlying medical conditions.
- Relief strategies:
- Increase fiber intake: Aim for 25-30 grams of fiber per day from sources like fruits, vegetables, and whole grains.
- Stay hydrated: Drink plenty of water throughout the day.
- Engage in regular physical activity: Exercise can help stimulate bowel movements.
- Consider over-the-counter remedies: Stool softeners or osmotic laxatives can provide temporary relief.
5.2. Diarrhea: Causes and Management
Diarrhea is characterized by frequent, loose, and watery stools.
- Common causes: Infections, food poisoning, medication side effects, food intolerances, and inflammatory bowel diseases.
- Management strategies:
- Stay hydrated: Drink plenty of fluids to replace lost electrolytes.
- Eat easily digestible foods: Follow the BRAT diet (bananas, rice, applesauce, toast).
- Avoid dairy products, caffeine, and sugary drinks: These can worsen diarrhea.
- Consider over-the-counter remedies: Anti-diarrheal medications can provide temporary relief.
5.3. Irritable Bowel Syndrome (IBS): Symptoms and Management
IBS is a chronic disorder that affects the large intestine, causing symptoms such as abdominal pain, bloating, gas, diarrhea, and constipation.
- Common symptoms: Abdominal pain, bloating, gas, diarrhea, and constipation.
- Management strategies:
- Dietary modifications: Identify and avoid trigger foods.
- Stress management: Practice relaxation techniques such as yoga, meditation, or deep breathing exercises.
- Medications: Certain medications can help relieve specific symptoms such as abdominal pain or diarrhea.
5.4. Acid Reflux and Heartburn: Causes and Relief
Acid reflux occurs when stomach acid flows back into the esophagus, causing symptoms such as heartburn, regurgitation, and chest pain.
- Common causes: Overeating, lying down after meals, obesity, pregnancy, and certain medications.
- Relief strategies:
- Eat smaller, more frequent meals: Avoid overeating.
- Avoid trigger foods: Spicy, fatty, and acidic foods can worsen acid reflux.
- Stay upright after meals: Avoid lying down for at least 2-3 hours after eating.
- Elevate the head of your bed: This can help prevent stomach acid from flowing back into the esophagus.
- Consider over-the-counter remedies: Antacids can provide temporary relief.
6. How Diet Affects Digestion and Feces Formation
What you eat significantly impacts your digestion and the formation of feces. Understanding the role of different food components can help you make healthier choices.
6.1. The Role of Fiber: Soluble vs. Insoluble
Fiber is a type of carbohydrate that the body cannot digest. It adds bulk to the stool, promotes regular bowel movements, and helps to regulate blood sugar and cholesterol levels.
- Soluble fiber: Dissolves in water and forms a gel-like substance in the digestive tract. It helps to lower cholesterol levels and regulate blood sugar.
- Insoluble fiber: Does not dissolve in water and adds bulk to the stool, promoting regular bowel movements.
- Good sources of fiber: Fruits, vegetables, whole grains, legumes, and nuts.
6.2. Hydration: Importance of Water Intake
Water is essential for digestion and feces formation. It helps to soften the stool, making it easier to pass, and prevents constipation.
- Recommended water intake: Aim for at least 8 cups of water per day.
- Sources of hydration: Water, fruits, vegetables, and other beverages.
- Dehydration symptoms: Constipation, fatigue, headache, and dizziness.
6.3. Impact of Processed Foods: Additives and Preservatives
Processed foods often contain additives and preservatives that can negatively impact digestion and gut health.
- Harmful additives: Artificial sweeteners, emulsifiers, and preservatives can disrupt the gut microbiome and promote inflammation.
- Reduced nutrient content: Processed foods are often low in fiber, vitamins, and minerals, which are essential for digestive health.
- Healthier alternatives: Choose whole, unprocessed foods whenever possible.
6.4. Probiotics and Prebiotics: Supporting Gut Health
Probiotics are beneficial bacteria that can improve gut health. Prebiotics are non-digestible fibers that feed these bacteria.
- Probiotic sources: Yogurt, kefir, sauerkraut, kimchi, and supplements.
- Prebiotic sources: Garlic, onions, leeks, asparagus, and bananas.
- Benefits of probiotics and prebiotics: Improved digestion, enhanced immunity, and a reduced risk of chronic diseases.
7. How Exercise and Physical Activity Impact Digestion
Physical activity plays a vital role in promoting healthy digestion. Regular exercise can stimulate bowel movements, reduce stress, and improve overall gut health.
7.1. Stimulating Bowel Movements
Exercise can help stimulate bowel movements by increasing blood flow to the digestive tract and strengthening the muscles involved in defecation.
- Types of exercise: Aerobic exercises such as walking, running, and swimming are particularly effective.
- Frequency and duration: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Consistency: Regular exercise is more effective than sporadic bursts of activity.
7.2. Reducing Stress and Anxiety
Stress and anxiety can negatively impact digestion, leading to symptoms such as abdominal pain, bloating, and changes in bowel habits.
- Stress-reducing exercises: Yoga, tai chi, and meditation can help reduce stress and improve digestion.
- Mind-body connection: Paying attention to your body and practicing mindfulness can help you identify and manage stress triggers.
- Overall well-being: Regular exercise can improve mood, reduce anxiety, and promote overall well-being, all of which can benefit digestion.
7.3. Improving Gut Motility
Gut motility refers to the movement of food through the digestive tract. Exercise can help improve gut motility by strengthening the muscles of the digestive system and promoting regular contractions.
- Strengthening abdominal muscles: Exercises such as sit-ups, crunches, and planks can help strengthen the abdominal muscles, which play a role in gut motility.
- Promoting regular contractions: Aerobic exercise can stimulate peristalsis, the rhythmic contractions that move food through the digestive tract.
- Preventing constipation: By improving gut motility, exercise can help prevent constipation and promote regular bowel movements.
8. Food Intolerances and Sensitivities
Food intolerances and sensitivities can cause digestive symptoms such as bloating, gas, abdominal pain, and diarrhea. Identifying and avoiding these foods can significantly improve your digestive health.
8.1. Lactose Intolerance: Symptoms and Management
Lactose intolerance is a common condition in which the body is unable to digest lactose, a sugar found in dairy products.
- Common symptoms: Bloating, gas, abdominal pain, and diarrhea after consuming dairy products.
- Management strategies:
- Limit dairy intake: Reduce your consumption of dairy products.
- Choose lactose-free products: Opt for lactose-free milk, yogurt, and cheese.
- Take lactase supplements: These supplements can help you digest lactose.
8.2. Gluten Sensitivity: Symptoms and Management
Gluten sensitivity, also known as non-celiac gluten sensitivity (NCGS), is a condition in which the body reacts negatively to gluten, a protein found in wheat, barley, and rye.
- Common symptoms: Bloating, abdominal pain, fatigue, headache, and skin rashes after consuming gluten-containing foods.
- Management strategies:
- Follow a gluten-free diet: Avoid wheat, barley, and rye.
- Read food labels carefully: Gluten can be found in unexpected places.
- Choose gluten-free alternatives: Opt for gluten-free bread, pasta, and other products.
8.3. FODMAPs: Understanding and Managing Them
FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are a group of carbohydrates that can cause digestive symptoms in some people.
- Common symptoms: Bloating, gas, abdominal pain, and diarrhea after consuming high-FODMAP foods.
- Management strategies:
- Follow a low-FODMAP diet: Avoid high-FODMAP foods such as garlic, onions, apples, pears, and dairy products.
- Work with a registered dietitian: A dietitian can help you identify your specific FODMAP triggers and develop a personalized meal plan.
- Reintroduce foods gradually: After a period of elimination, you can gradually reintroduce FODMAPs to determine your tolerance level.
9. When to See a Doctor: Red Flags
While many digestive issues can be managed with lifestyle changes and over-the-counter remedies, certain symptoms warrant medical attention.
9.1. Persistent Abdominal Pain
Persistent abdominal pain that does not improve with home remedies should be evaluated by a doctor.
- Possible causes: Appendicitis, gallstones, pancreatitis, inflammatory bowel disease, or cancer.
- Importance of early diagnosis: Early diagnosis and treatment can improve outcomes and prevent complications.
9.2. Unexplained Weight Loss
Unexplained weight loss, especially if accompanied by other symptoms such as fatigue or abdominal pain, should be evaluated by a doctor.
- Possible causes: Cancer, inflammatory bowel disease, hyperthyroidism, or malabsorption.
- Importance of thorough evaluation: A thorough medical evaluation can help identify the underlying cause of weight loss.
9.3. Blood in Stool
Blood in the stool can be a sign of a serious medical condition and should be evaluated by a doctor.
- Possible causes: Hemorrhoids, anal fissures, inflammatory bowel disease, or cancer.
- Importance of prompt evaluation: Prompt evaluation can help determine the cause of bleeding and initiate appropriate treatment.
9.4. Changes in Bowel Habits
Sudden and persistent changes in bowel habits, such as diarrhea or constipation, should be evaluated by a doctor.
- Possible causes: Infections, inflammatory bowel disease, irritable bowel syndrome, or cancer.
- Importance of monitoring: Monitoring changes in bowel habits can help detect potential problems early.
10. Expert Tips for a Healthy Digestive System
Maintaining a healthy digestive system involves a combination of dietary choices, lifestyle habits, and proactive management.
10.1. Mindful Eating Practices
Mindful eating involves paying attention to your food and eating with intention.
- Benefits: Improved digestion, increased satiety, and reduced overeating.
- Techniques:
- Eat slowly: Take your time and savor each bite.
- Eliminate distractions: Turn off the TV and put away your phone.
- Pay attention to your body: Notice when you’re full and stop eating.
10.2. Stress Management Techniques
Stress can negatively impact digestion, so managing stress is essential for gut health.
- Effective techniques:
- Yoga: Combines physical postures, breathing exercises, and meditation.
- Meditation: Focuses on quieting the mind and promoting relaxation.
- Deep breathing exercises: Can help calm the nervous system and reduce stress.
- Spending time in nature: Can have a calming and restorative effect.
10.3. Regular Exercise Routine
Regular physical activity can improve digestion, reduce stress, and promote overall well-being.
- Recommended activities:
- Walking: A low-impact exercise that can be easily incorporated into your daily routine.
- Running: A more intense aerobic exercise that can improve cardiovascular health and digestion.
- Swimming: A full-body workout that is gentle on the joints.
- Yoga: Combines physical postures, breathing exercises, and meditation.
10.4. Consistent Sleep Schedule
Getting enough sleep is essential for overall health, including digestive health.
- Recommended sleep duration: Aim for 7-9 hours of sleep per night.
- Tips for better sleep:
- Establish a regular sleep schedule: Go to bed and wake up at the same time each day.
- Create a relaxing bedtime routine: Take a warm bath, read a book, or listen to calming music.
- Avoid caffeine and alcohol before bed: These substances can interfere with sleep.
- Create a dark, quiet, and cool sleep environment.
Understanding how food turns into feces is fundamental to appreciating the intricate workings of our bodies. By making informed choices about diet, exercise, and lifestyle, we can optimize our digestive health and overall well-being.
For more in-depth information and expert guidance on digestive health, visit FOODS.EDU.VN, where you’ll find a wealth of articles, recipes, and resources to support your journey to a healthier you. Our team of experts provides reliable, evidence-based information to help you make the best choices for your digestive health.
- Address: 1946 Campus Dr, Hyde Park, NY 12538, United States
- WhatsApp: +1 845-452-9600
- Website: FOODS.EDU.VN
Discover the secrets to a happy gut and a healthier life with foods.edu.vn! Let us help you unlock the full potential of your digestive system, leading to improved energy, better nutrient absorption, and a greater sense of well-being. Visit us today and embark on a journey to optimal digestive health.
FAQ: How Food Becomes Feces
1. How long does it take for food to turn into feces?
The entire digestive process, from eating to elimination, typically takes between 24 to 72 hours. This can vary depending on factors such as diet, metabolism, and individual digestive health.
2. What happens if food passes through the digestive system too quickly?
If food passes through the digestive system too quickly, such as in cases of diarrhea, there may not be enough time for water and nutrients to be properly absorbed. This can lead to dehydration and nutrient deficiencies.
3. What happens if food stays in the digestive system for too long?
If food stays in the digestive system for too long, such as in cases of constipation, too much water may be absorbed, resulting in hard, difficult-to-pass stools. This can lead to discomfort and other complications.
4. What is the role of the appendix in digestion?
The appendix is a small, finger-like pouch that extends from the large intestine. While it was once thought to be a vestigial organ with no function, it is now believed to play a role in immune function and maintaining a healthy gut microbiome.
5. How does stress affect digestion and feces formation?
Stress can have a significant impact on digestion and feces formation. It can disrupt the gut microbiome, alter gut motility, and increase inflammation, leading to symptoms such as abdominal pain, bloating, diarrhea, or constipation.
6. Can certain medications affect the digestive process?
Yes, certain medications can affect the digestive process. For example, antibiotics can disrupt the gut microbiome, while pain relievers can cause constipation. It’s important to be aware of the potential side effects of medications and discuss any concerns with your doctor.
7. What are some foods that promote healthy bowel movements?
Foods that are high in fiber, such as fruits, vegetables, whole grains, and legumes, can promote healthy bowel movements. Probiotic-rich foods, such as yogurt and kefir, can also support a healthy gut microbiome and regular bowel habits.
8. How can I improve my digestive health naturally?
You can improve your digestive health naturally by eating a balanced diet, staying hydrated, exercising regularly, managing stress, and getting enough sleep. You may also consider adding probiotic-rich foods or supplements to your diet.
9. Is it normal to have gas after eating?
It is normal to have gas after eating, as gas is a byproduct of the digestion process. However, excessive gas, bloating, or abdominal pain may indicate a digestive issue.
10. What is the difference between a food allergy and a food intolerance?
A food allergy is an immune system response to a specific food, while a food intolerance is a digestive issue that does not involve the immune system. Food allergies can cause severe reactions, while food intolerances typically cause digestive symptoms such as bloating, gas, or diarrhea.