Are you curious about What Is Histamine In Food and its impact on your health? FOODS.EDU.VN offers insights into histamine, a natural compound found in various foods. Understanding histamine levels and their effects can help manage sensitivities and improve your overall well-being. Discover expert advice and practical tips on FOODS.EDU.VN today. Explore the world of histamine intolerance and its related dietary concerns, from histamine-rich foods to low-histamine diets, all in one place.
1. Understanding Histamine: A Deep Dive
Histamine, a biogenic amine derived from the amino acid L-histidine, plays a multifaceted role in the human body. While often associated with allergic reactions, it’s also crucial for various physiological processes. This section delves into the nature of histamine, its formation, and its significance.
1.1. What is Histamine?
Histamine (2-[4-imidazole]-ethylamine) acts as a key regulator in the body. It forms from L-histidine through the action of L-histidine decarboxylase, an enzyme present in nearly all organs and tissues, using vitamin B6 (pyridoxal phosphate) as a co-factor [21]. This process happens both within our bodies and in foods, particularly those undergoing fermentation or spoilage.
1.2. How is Histamine Formed?
The production of histamine primarily occurs through the enzymatic decarboxylation of histidine. Bacteria and human decarboxylases activate when there’s an increased demand for histamine, such as regulating intraplasmic pH under conditions of lactic acidosis [22]. This process is essential in various physiological and pathological conditions, highlighting histamine’s adaptability.
1.3. Histamine’s Role in the Body
Histamine is stored mainly in microsomes and the nucleus within cells. Nuclear chromatin shows a high affinity for histamine, which decreases during active DNA division, like regeneration [22]. Mast cells and basophils store significant amounts of histamine in their endoplasmic granules, playing a regulatory role that, when disrupted, can lead to unpredictable consequences [23].
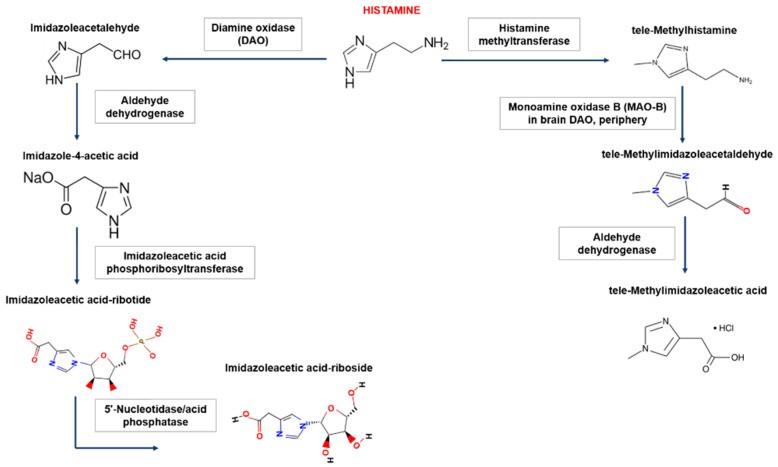
2. Histamine Metabolism: How Your Body Handles It
The body has two primary pathways for breaking down histamine: diamine oxidase (DAO) and histamine-N-methyltransferase (HNMT). Understanding these pathways is key to grasping histamine intolerance.
2.1. The Role of Diamine Oxidase (DAO)
DAO, mainly synthesized in the mucous membrane of the small and ascending colon, the placenta, and the kidneys, degrades extracellular histamine. It acts as a “barrier function,” limiting histamine passage from the intestines into the blood [24].
2.2. Histamine-N-Methyltransferase (HNMT) Function
HNMT methylates histamine inside cells, using B vitamins and S-adenosylmethionine [24]. This enzyme is present in most tissues and regulates intracellular histamine content, with high activity in the kidneys, liver, spleen, colon, and more.
2.3. Genetic Factors in Histamine Metabolism
Polymorphisms in the DAO and HNMT genes can lead to individual differences in histamine metabolism. Synaptic acetaldehyde dehydrogenase also plays a role in histamine degradation [20].
3. Histamine Intolerance: Causes and Symptoms
Histamine intolerance, also known as enteric histaminosis or dietary histamine sensitivity, arises from the body’s impaired ability to metabolize histamine effectively [24]. This imbalance can lead to a variety of uncomfortable symptoms.
3.1. What Causes Histamine Intolerance?
Food histamine enters the body through the intestinal epithelium, with DAO playing a crucial role in metabolizing exogenous histamine from food and microbiota [18,25,26]. Insufficient DAO activity or factors reducing it can lead to histaminosis [18,25,26,27].
3.2. Factors Increasing Histamine Levels
Histamine levels in the intestinal lumen can increase not only from oral consumption but also from histidine decarboxylation from hemoglobin during gastrointestinal bleeding or intestinal obstruction. Highly active histidine decarboxylases in the microbiota are also significant contributors [29,30].
3.3. Common Symptoms of Histamine Intolerance
Symptoms are diverse and non-specific due to the widespread distribution of histamine receptors. Common manifestations include gastrointestinal issues like bloating, diarrhea, abdominal pain, and constipation. Neurological and cardiovascular symptoms such as dizziness, headaches, and palpitations, as well as respiratory and dermatological symptoms, are also frequent [80].
4. Foods High in Histamine: What to Avoid
Certain foods naturally contain high levels of histamine or can trigger its release in the body. Identifying these foods is crucial for managing histamine intolerance.
4.1. List of High-Histamine Foods
Foods high in histamine include:
- Fermented foods: Cheese, sauerkraut, kimchi, yogurt, kefir
- Alcohol: Especially wine and beer
- Processed meats: Smoked meats, sausages, salami
- Certain fish: Mackerel, tuna, anchovies
- Vegetables: Eggplant, spinach, tomatoes
- Fruits: Citrus fruits, strawberries, bananas
- Vinegar-containing foods: Pickles, mayonnaise, ketchup
4.2. How Storage Affects Histamine Levels
The way food is stored significantly impacts histamine levels. High-protein foods like fish and meat stored in unsuitable conditions or contaminated with microorganisms accumulate histamine. Histidine decarboxylase, the enzyme converting histidine to histamine, remains active even at low temperatures and reactivates after thawing [70].
4.3. Foods That Release Histamine (Histamine Liberators)
Some foods don’t contain high levels of histamine but can trigger its release in the body. These histamine liberators include:
- Citrus fruits
- Strawberries
- Tomatoes
- Chocolate
- Alcohol
- Certain spices
5. Low-Histamine Diet: A Guide
Adopting a low-histamine diet can significantly alleviate symptoms of histamine intolerance. This involves carefully selecting foods and being mindful of storage and preparation methods.
5.1. What is a Low-Histamine Diet?
A low-histamine diet focuses on consuming fresh, unprocessed foods that are naturally low in histamine. It requires avoiding high-histamine foods and histamine liberators to reduce the overall histamine load on the body.
5.2. Foods to Include in a Low-Histamine Diet
- Freshly cooked meats and poultry
- Fresh fish (quickly frozen after catch)
- Most fresh fruits (excluding strawberries, citrus)
- Most fresh vegetables (excluding tomatoes, spinach, eggplant)
- Rice, corn, and other grains
- Dairy substitutes: Rice milk, coconut milk
5.3. Tips for Following a Low-Histamine Diet
- Eat Fresh: Consume freshly prepared foods immediately.
- Avoid Leftovers: Histamine levels increase as food sits.
- Cook Simply: Opt for simple cooking methods to avoid added histamine.
- Read Labels: Be vigilant about ingredients in packaged foods.
- Keep a Food Diary: Track your meals and symptoms to identify trigger foods.
6. Diagnosing Histamine Intolerance: What to Expect
Diagnosing histamine intolerance can be challenging due to its non-specific symptoms. However, a systematic approach can help identify the condition.
6.1. Diagnostic Steps
According to the World Allergy Organization’s 2003 recommendations, diagnosing non-immunological reactions to food involves several stages [83]:
Stage 1: Rule out IgE-mediated allergic reactions using skin tests, systemic mastocytosis by studying serum tryptase activity, and evaluate concomitant digestive system diseases. Assess medical history for medications inhibiting DAO.
Stage 2: Adhere to a low-histamine diet for 4–8 weeks, monitoring the dynamics of symptoms. A decrease in symptoms suggests histamine intolerance.
Stage 3: Laboratory diagnostics, including DAO activity in blood serum or intestinal biopsy, oral histamine challenge test, skin prick test with histamine, DAO genetic polymorphism research, and analysis of histamine metabolites in urine and feces.
6.2. Testing for DAO Activity
Measuring DAO activity in blood serum is a common diagnostic test. A threshold value below 10 U/mL suggests a high likelihood of histamine intolerance, but DAO activity can vary significantly, so results should be interpreted with caution [24,84].
6.3. Other Diagnostic Tests
Other tests include histamine skin prick tests, oral histamine challenge tests, and measuring urinary histamine metabolites. Oral histamine challenges carry risks and should be performed in a hospital setting, and potentiating factors like alcohol and biogenic amines should be considered [24].
7. Medications and Supplements for Histamine Intolerance
In addition to dietary changes, certain medications and supplements can help manage histamine intolerance symptoms.
7.1. Antihistamines: H1 and H2 Blockers
H1 receptor antagonists, like ebastine (Kestin®), have shown effectiveness in clinical remission for IBS-D patients. H2 blockers, however, have not been as effective [93,114,122].
7.2. DAO Supplements: How They Help
DAO-containing food additives, based on enteric-coated pig kidney extracts, can help increase the gut’s ability to eliminate histamine from food. Legume sprouts are also a source of DAO, with enzyme activity 250-fold higher than non-sprouted seeds. Supplementation with DAO has been shown to improve the quality of life for patients with histamine intolerance [120].
7.3. Other Supplements
- Vitamin C: Enhances histamine degradation and inhibits mast cell degranulation [127].
- Quercetin: A natural flavonoid that inhibits mast cell degranulation in vitro [128].
- Probiotics: Certain strains like L. faecalis can help degrade histamine.
8. Histamine Receptors: How They Work
Histamine exerts its effects by binding to four types of receptors: H1, H2, H3, and H4. Each receptor plays a different role in the body.
8.1. H1 Receptors
H1Rs are present in the endothelium and vascular smooth muscle cells, particularly in the gastrointestinal tract, hypothalamus, adrenal medulla, and immunocompetent cells. Stimulation leads to inflammation, vasodilation, increased vascular permeability, and bronchoconstriction [42].
8.2. H2 Receptors
H2Rs are found in parietal cells of the stomach, enterocytes, endothelium, and immunocompetent cells. Stimulation leads to external secretion (primarily hydrochloric acid), tachycardia, and relaxation of smooth muscle cells [42].
8.3. H3 Receptors
H3Rs are located in the central nervous system and regulate the release of neurotransmitters like acetylcholine, serotonin, and norepinephrine. Changes in H3R activity can affect sleep, attention, and cognitive function [59].
8.4. H4 Receptors
H4Rs are mainly present on immune cells, leukocytes, mast cells, and in the intestinal epithelium. They are involved in inflammation and hypersensitivity reactions [64,65].
9. Mast Cells and Histamine Release
Mast cells are critical players in histamine release. Understanding their function is essential for managing histamine-related conditions.
9.1. What are Mast Cells?
Mast cells are found in mucous and epithelial tissues throughout the body, particularly at the interface between the host and the external environment, such as the gastrointestinal tract, skin, and respiratory epithelium [88]. They store inflammatory mediators like histamine, tryptase, and interleukins [89].
9.2. How Mast Cells Release Histamine
Mast cells release histamine through “anaphylactic degranulation” when IgE interacts with the FcRI receptor and allergen. They also express IgG receptors, complement receptors, and pattern recognition receptors, leading to “marginal degranulation” under certain conditions [92].
9.3. Factors Affecting Mast Cell Activation
Several factors can affect mast cell activation, including bacterial infections, hormones, neurotransmitters, and certain drugs like fluoroquinolones. The intestinal microbiota and the functional state of intestinal nerves also play significant roles [92,102].
10. Related Conditions: IBS and Histamine
Histamine intolerance can be linked to other conditions, such as irritable bowel syndrome (IBS). Exploring these connections can help in comprehensive management.
10.1. The Link Between Histamine and IBS
In many patients with functional dyspepsia and irritable bowel syndrome with diarrhea (IBS-D), hyperplasia and increased activity of mast cells are observed, linked to increased neuron excitability and intestinal permeability [92,109,110,111,[112](#B112-nutrients-13-03207],[113](#B113-nutrients-13-03207]].
10.2. Managing IBS with Histamine Intolerance
Managing IBS with histamine intolerance involves a low-histamine diet, histamine receptor blockers, mast cell membrane stabilizers, and addressing any underlying conditions or triggers [24].
10.3. Dietary Considerations for IBS and Histamine
Dietary considerations include avoiding high-FODMAP foods, which can exacerbate IBS symptoms, in addition to following a low-histamine diet to minimize histamine-related issues [121].
11. Practical Tips for Reducing Histamine Intake
Reducing histamine intake involves making informed food choices and adopting specific lifestyle habits.
11.1. Shopping Strategies
- Buy Fresh: Purchase fresh produce, meat, and fish.
- Check Labels: Look for preservatives and additives that may increase histamine.
- Shop Frequently: Reduce the need to store food for extended periods.
11.2. Cooking and Preparation Techniques
- Cook Immediately: Prepare and cook food as soon as possible after purchase.
- Avoid Fermentation: Steer clear of fermented or aged products.
- Simple Recipes: Choose recipes with minimal ingredients and processing.
11.3. Lifestyle Adjustments
- Manage Stress: High stress levels can exacerbate histamine-related symptoms.
- Stay Hydrated: Drink plenty of water to support histamine metabolism.
- Avoid Alcohol: Alcohol can inhibit DAO activity and increase histamine release.
12. The Future of Histamine Intolerance Research
Ongoing research continues to shed light on histamine intolerance, offering hope for better diagnostic tools and treatment strategies.
12.1. Current Research Trends
Current research focuses on identifying new sources of DAO enzymes, understanding the role of gut microbiota, and developing more effective histamine receptor blockers [24].
12.2. Potential Breakthroughs
Potential breakthroughs include developing plant-based DAO supplements, personalized probiotic therapies, and targeted treatments for mast cell activation syndrome [24].
12.3. The Role of Personalized Nutrition
Personalized nutrition, tailored to individual genetic and metabolic profiles, may offer the most effective approach for managing histamine intolerance in the future [24].
FAQ: Your Questions Answered about Histamine in Food
1. What exactly is histamine?
Histamine is a natural amine derived from L-histidine, playing roles in immune responses, gastric acid secretion, and neurotransmission.
2. What foods are highest in histamine?
High-histamine foods include fermented products, aged cheeses, processed meats, and certain fish.
3. How does histamine intolerance differ from a food allergy?
Histamine intolerance is a non-allergic food intolerance due to impaired histamine metabolism, unlike food allergies involving immune responses.
4. Can histamine levels in food be reduced?
Yes, by consuming fresh foods immediately after preparation and avoiding leftovers.
5. What are the symptoms of histamine intolerance?
Symptoms include bloating, diarrhea, headaches, skin rashes, and cardiovascular issues.
6. How is histamine intolerance diagnosed?
Diagnosis involves symptom assessment, dietary elimination, and tests for DAO activity.
7. What is a low-histamine diet?
A low-histamine diet involves avoiding high-histamine foods and histamine liberators.
8. Can supplements help with histamine intolerance?
Yes, DAO supplements, Vitamin C, and Quercetin can help manage symptoms.
9. Is histamine intolerance related to IBS?
Yes, histamine intolerance can exacerbate IBS symptoms due to mast cell activation.
10. Where can I find more information about histamine in food?
Explore FOODS.EDU.VN for detailed guides, recipes, and expert advice on managing histamine intolerance.
In conclusion, understanding what is histamine in food and how it affects your body is essential for managing histamine intolerance. By following a low-histamine diet, adopting practical tips, and seeking appropriate medical advice, you can alleviate symptoms and improve your quality of life. For more in-depth information and resources, visit FOODS.EDU.VN, your trusted source for comprehensive food and nutrition knowledge.
Are you ready to take control of your health and explore the world of low-histamine eating? Visit FOODS.EDU.VN today for detailed recipes, expert tips, and a supportive community to help you navigate histamine intolerance with confidence. Discover a wealth of knowledge and resources that empower you to make informed choices and live a healthier, happier life. Don’t let histamine intolerance hold you back—unlock your potential with foods.edu.vn. Contact us at 1946 Campus Dr, Hyde Park, NY 12538, United States. Whatsapp: +1 845-452-9600.
Image depicting the biogenic amine histamine metabolism process within the human body, highlighting how histamine is metabolized via diamine oxidase (DAO) and histamine N-methyltransferase enzymes.
Visual representation of the biological effects of histamine receptors, showcasing the H1-H4 receptor subtypes and their varied roles in immune response, vasodilation, gastric acid secretion, and neurotransmission.