A food coma, also known as postprandial somnolence, is that feeling of sleepiness and lethargy that hits you after a large meal; FOODS.EDU.VN can help you understand why. This occurs due to physiological changes as your body digests a significant amount of food, leading to that all-too-familiar urge to nap, and exploring the causes, symptoms, and ways to mitigate this common experience can help you enjoy your meals without the subsequent slump, and also learn more about metabolic slowdown and digestive slowdown.
1. Defining the Food Coma: Postprandial Somnolence Explained
What exactly is a food coma? Postprandial somnolence, colloquially known as a food coma, is the state of drowsiness or lethargy that occurs after eating a large meal. This condition is a common physiological response to the digestive process, particularly after consuming meals high in carbohydrates and fats. It’s not a true coma in the medical sense, but rather a temporary state of reduced alertness and energy. The term “food coma” emerged in the 1980s to describe this widespread experience of post-meal fatigue. Understanding the physiological mechanisms behind postprandial somnolence can help individuals make informed dietary choices and lifestyle adjustments to minimize its effects.
1.1. The Science Behind Postprandial Somnolence
The underlying causes of a food coma are multifaceted, involving hormonal changes, blood flow redistribution, and neural signaling. Here’s a detailed look at the key factors:
- Increased Blood Flow to the Digestive System: After a large meal, the body diverts a significant amount of blood flow to the gastrointestinal tract to aid in digestion and nutrient absorption. This shift in blood flow reduces blood supply to other areas of the body, including the brain, which can lead to feelings of fatigue and reduced mental alertness.
- Hormonal Responses: The consumption of food triggers the release of various hormones that play a role in digestion and metabolism. For instance, the hormone cholecystokinin (CCK) is released in response to fats and proteins, promoting satiety and slowing gastric emptying. This can contribute to feelings of fullness and drowsiness.
- Insulin and Blood Sugar Levels: Carbohydrate-rich meals can cause a rapid increase in blood sugar levels, prompting the pancreas to release insulin to facilitate glucose uptake by cells. This rapid fluctuation in blood sugar can lead to an initial energy surge followed by a subsequent crash, contributing to the sensation of a food coma.
- Vagus Nerve Activation: The vagus nerve, a major component of the parasympathetic nervous system, plays a crucial role in regulating digestion. Activation of the vagus nerve promotes relaxation and reduces heart rate, which can contribute to the sedative effects experienced after eating.
1.2. What Contributes to Food Coma?
Several factors can influence the likelihood and severity of experiencing a food coma:
- Meal Size: Larger meals require more energy for digestion, increasing the metabolic burden on the body and the likelihood of experiencing postprandial somnolence.
- Macronutrient Composition: Meals high in carbohydrates and fats are more likely to induce a food coma compared to meals with a balanced macronutrient profile. Carbohydrates, especially simple sugars, can cause rapid spikes and crashes in blood sugar levels, while fats are more energy-dense and require longer digestion times.
- Individual Metabolism: Metabolic rate, insulin sensitivity, and digestive efficiency vary among individuals, influencing how the body processes food and the subsequent impact on energy levels.
- Time of Day: Circadian rhythms influence energy levels throughout the day. Eating a large meal during a time when the body is naturally inclined to rest (e.g., afternoon) can exacerbate the effects of postprandial somnolence.
- Pre-existing Conditions: Individuals with certain medical conditions, such as diabetes or insulin resistance, may be more susceptible to experiencing pronounced food comas due to impaired glucose metabolism.
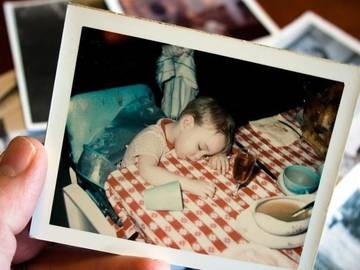 Man asleep on couch after eating
Man asleep on couch after eating
2. Common Symptoms of a Food Coma
What are the typical signs that you’re experiencing a food coma? The symptoms of a food coma can range from mild to severe, depending on the individual and the characteristics of the meal. Recognizing these symptoms can help you anticipate and manage postprandial somnolence effectively.
2.1. Key Symptoms to Watch For
Here are the most common symptoms associated with a food coma:
- Sleepiness and Drowsiness: This is the hallmark symptom of a food coma. You may feel an overwhelming urge to nap or close your eyes.
- Lethargy and Fatigue: A general feeling of sluggishness and reduced energy levels. Simple tasks may seem more difficult to accomplish.
- Reduced Mental Alertness: Difficulty concentrating, thinking clearly, or making decisions. Cognitive functions may feel temporarily impaired.
- Heaviness and Fullness: A sensation of being overly full and uncomfortable, often accompanied by bloating or distension.
- Decreased Motivation: A lack of enthusiasm for activities and a desire to rest or relax.
- Mild Cognitive Impairment: Some individuals may experience mild memory lapses or difficulty recalling information.
- Physical Discomfort: In some cases, food comas can be accompanied by physical discomfort such as heartburn, nausea, or abdominal cramping.
2.2. Understanding the Impact on Daily Activities
The symptoms of a food coma can significantly impact daily activities and productivity. Reduced mental alertness and fatigue can make it challenging to perform tasks that require focus and concentration, such as studying, working, or driving. The physical discomfort associated with a food coma can also make it difficult to engage in physical activities or social interactions.
3. The Role of Tryptophan: Debunking the Turkey Myth
Does turkey actually make you sleepy? The common belief that turkey is the primary culprit behind post-Thanksgiving dinner drowsiness is largely a myth. While turkey does contain tryptophan, an amino acid associated with sleepiness, it’s not the sole cause of a food coma.
3.1. Tryptophan’s Function and Effects
Tryptophan is an essential amino acid that the body uses to produce serotonin and melatonin, neurotransmitters that regulate mood and sleep. Serotonin helps to stabilize mood and promote feelings of well-being, while melatonin helps to regulate the sleep-wake cycle.
3.2. Why Turkey Isn’t the Only Culprit
While turkey contains tryptophan, the amount is not significantly higher than in other common protein sources such as chicken, beef, nuts, eggs, or cheese. Several other factors contribute to the drowsiness experienced after a Thanksgiving meal:
- Large Meal Size: The sheer volume of food consumed during a Thanksgiving dinner places a significant burden on the digestive system.
- Carbohydrate-Rich Sides: The abundance of carbohydrate-rich side dishes, such as mashed potatoes, stuffing, and sweet potato casserole, can lead to rapid spikes and crashes in blood sugar levels.
- Alcohol Consumption: Alcohol can enhance the sedative effects of a food coma.
- Relaxed Environment: The relaxed and festive atmosphere of Thanksgiving can contribute to feelings of drowsiness and relaxation.
4. Foods That Can Induce a Food Coma
What types of foods are most likely to cause a food coma? Certain types of foods are more likely to induce postprandial somnolence due to their macronutrient composition and impact on blood sugar levels. Here’s a breakdown of the common culprits:
4.1. High-Carbohydrate Foods
Foods high in carbohydrates, especially simple sugars and refined grains, can cause rapid spikes and crashes in blood sugar levels, leading to energy fluctuations and fatigue.
- Pastries and Desserts: Cakes, cookies, pies, and other sweet treats are loaded with sugar and refined flour, which can trigger a rapid insulin response and subsequent energy crash.
- Examples: Apple pie, chocolate cake, doughnuts
- Impact: Quick energy boost followed by a sharp decline, contributing to drowsiness
- White Bread and Pasta: Refined grains are quickly digested, leading to a rapid increase in blood sugar levels.
- Examples: White bread, pasta, and bagels
- Impact: Similar to pastries, these can cause energy spikes and crashes
- Sugary Drinks: Sodas, fruit juices, and sweetened beverages can cause a rapid increase in blood sugar levels.
- Examples: Soda, juice, sweetened tea
- Impact: Rapid sugar absorption leads to energy fluctuations
4.2. High-Fat Foods
Foods high in fat require more energy to digest and can slow down gastric emptying, leading to feelings of fullness and lethargy.
- Fried Foods: French fries, fried chicken, and other fried foods are high in both fat and calories, which can take a toll on the digestive system.
- Examples: French fries, fried chicken, and onion rings
- Impact: Slow digestion and sustained feelings of fullness
- Rich Sauces and Gravies: Cream-based sauces and gravies are high in fat and can contribute to feelings of fullness and drowsiness.
- Examples: Alfredo sauce, creamy gravy
- Impact: Increased fat content can slow down digestion
- Fatty Meats: High-fat cuts of meat, such as bacon and sausage, can be difficult to digest and contribute to lethargy.
- Examples: Bacon, sausage, and fatty steaks
- Impact: Higher fat content requires more energy to digest
4.3. Large Meals
Consuming large quantities of food, regardless of macronutrient composition, can place a significant burden on the digestive system and increase the likelihood of experiencing a food coma.
- Buffets: All-you-can-eat buffets often encourage overeating, leading to digestive distress and fatigue.
- Examples: Holiday buffets, all-you-can-eat restaurants
- Impact: Overconsumption strains the digestive system
- Holiday Feasts: Thanksgiving, Christmas, and other holiday celebrations often involve large, multi-course meals that can overwhelm the digestive system.
- Examples: Thanksgiving dinner, Christmas feast
- Impact: Combination of large portions and rich foods can induce a food coma
5. Foods That Help Prevent a Food Coma
Are there foods that can help prevent post-meal drowsiness? Yes, choosing foods that promote stable blood sugar levels and are easier to digest can help minimize the likelihood of experiencing a food coma.
5.1. High-Fiber Foods
Fiber-rich foods help to regulate blood sugar levels and promote digestive health.
- Vegetables: Leafy greens, broccoli, carrots, and other vegetables are packed with fiber and nutrients.
- Examples: Spinach, broccoli, and carrots
- Benefits: Slows down digestion and helps stabilize blood sugar
- Fruits: Apples, berries, and bananas are good sources of fiber and natural sugars.
- Examples: Apples, blueberries, bananas
- Benefits: Provides sustained energy without rapid spikes
- Whole Grains: Brown rice, quinoa, and oats are digested more slowly than refined grains, helping to stabilize blood sugar levels.
- Examples: Brown rice, quinoa, oatmeal
- Benefits: Sustained energy release and better blood sugar control
5.2. Lean Proteins
Lean protein sources provide sustained energy and help to balance blood sugar levels.
- Chicken and Turkey Breast: These lean protein sources are easy to digest and provide essential amino acids.
- Examples: Grilled chicken breast, roasted turkey breast
- Benefits: Provides sustained energy without rapid spikes
- Fish: Salmon, tuna, and other types of fish are rich in omega-3 fatty acids and protein.
- Examples: Salmon, tuna, cod
- Benefits: Healthy fats and proteins support stable energy levels
- Legumes: Beans, lentils, and chickpeas are good sources of protein and fiber.
- Examples: Lentils, chickpeas, black beans
- Benefits: Fiber and protein combination helps regulate blood sugar
5.3. Healthy Fats
Incorporating healthy fats into your meals can help to slow down digestion and promote satiety.
- Avocado: This creamy fruit is rich in healthy fats and fiber.
- Benefits: Promotes satiety and stable blood sugar
- Nuts and Seeds: Almonds, walnuts, chia seeds, and flaxseeds are good sources of healthy fats and nutrients.
- Benefits: Provides sustained energy and supports overall health
- Olive Oil: Using olive oil in cooking and salad dressings can provide healthy fats that help to slow down digestion.
- Benefits: Adds healthy fats to meals, promoting satiety
6. Practical Tips to Avoid a Food Coma
How can you prevent a food coma? Making simple changes to your eating habits and lifestyle can significantly reduce the likelihood and severity of postprandial somnolence.
6.1. Portion Control Strategies
Controlling portion sizes is crucial for preventing overeating and minimizing the burden on the digestive system.
- Use Smaller Plates: Using smaller plates can help you visually perceive a larger portion size, which can lead to eating less overall.
- Example: Switch from a 12-inch plate to a 9-inch plate
- Benefit: Reduces overall food intake
- Measure Food Portions: Accurately measuring food portions can help you stay within recommended serving sizes.
- Example: Use measuring cups and spoons
- Benefit: Prevents overeating by monitoring portion sizes
- Eat Slowly and Mindfully: Eating slowly allows your body to register fullness cues, which can prevent overeating.
- Example: Put your fork down between bites
- Benefit: Allows body to recognize satiety signals
6.2. Meal Timing and Frequency
Eating smaller, more frequent meals can help to stabilize blood sugar levels and prevent extreme energy fluctuations.
- Eat Every 3-4 Hours: Regular meals can help to keep blood sugar levels stable and prevent hunger-induced overeating.
- Example: Schedule meals and snacks throughout the day
- Benefit: Prevents large drops in blood sugar
- Avoid Skipping Meals: Skipping meals can lead to increased hunger and overeating later in the day.
- Example: Ensure consistent meal times
- Benefit: Prevents extreme hunger and overeating
- Limit Late-Night Eating: Eating large meals close to bedtime can interfere with sleep and contribute to postprandial somnolence.
- Example: Finish eating at least 3 hours before bed
- Benefit: Prevents digestive issues during sleep
6.3. Lifestyle Adjustments
Making certain lifestyle adjustments can also help to prevent food comas.
- Stay Hydrated: Drinking plenty of water can help to aid digestion and prevent dehydration-induced fatigue.
- Example: Carry a water bottle throughout the day
- Benefit: Supports digestion and prevents dehydration
- Engage in Light Exercise: Taking a short walk after eating can help to improve digestion and boost energy levels.
- Example: A 15-minute walk after meals
- Benefit: Improves digestion and energy levels
- Avoid Alcohol: Alcohol can enhance the sedative effects of a food coma, so it’s best to limit or avoid alcohol consumption with large meals.
- Example: Opt for non-alcoholic beverages
- Benefit: Reduces sedative effects
7. Medical Conditions and Food Comas
Are certain medical conditions linked to more intense food comas? Individuals with certain medical conditions may be more susceptible to experiencing pronounced food comas due to impaired metabolic function or other factors.
7.1. Diabetes and Insulin Resistance
Individuals with diabetes or insulin resistance may experience more severe food comas due to impaired glucose metabolism.
- Impaired Glucose Uptake: Insulin resistance can prevent cells from effectively taking up glucose from the bloodstream, leading to elevated blood sugar levels and subsequent energy crashes.
- Recommendation: Work with a healthcare provider to manage blood sugar levels
- Impact: More pronounced energy crashes after meals
- Increased Risk of Hyperglycemia: Individuals with diabetes are at risk of experiencing hyperglycemia (high blood sugar) after meals, which can lead to fatigue and other symptoms.
- Recommendation: Monitor blood sugar levels and adjust medication as needed
- Impact: Higher risk of fatigue and related symptoms
7.2. Digestive Disorders
Digestive disorders such as irritable bowel syndrome (IBS) and gastroparesis can also contribute to more pronounced food comas.
- IBS: IBS can cause digestive discomfort and altered bowel habits, which can be exacerbated by large meals.
- Recommendation: Identify and avoid trigger foods
- Impact: Increased digestive discomfort and fatigue
- Gastroparesis: Gastroparesis is a condition in which the stomach empties too slowly, leading to prolonged feelings of fullness and discomfort.
- Recommendation: Eat smaller, more frequent meals
- Impact: Prolonged fullness and discomfort
7.3. Food Allergies and Intolerances
Food allergies and intolerances can trigger inflammatory responses and digestive distress, which can contribute to fatigue and lethargy.
- Inflammatory Responses: Allergic reactions can trigger the release of inflammatory compounds that lead to fatigue and other systemic symptoms.
- Recommendation: Avoid known allergens
- Impact: Systemic inflammation and fatigue
- Digestive Distress: Food intolerances can cause bloating, gas, and other digestive symptoms that can interfere with energy levels.
- Recommendation: Identify and avoid problem foods
- Impact: Digestive discomfort and reduced energy
8. The Impact of a Food Coma on Cognitive Function
How does a food coma affect your brain? A food coma can have a significant impact on cognitive function, affecting concentration, memory, and overall mental performance.
8.1. Reduced Alertness and Concentration
One of the most noticeable effects of a food coma is reduced alertness and difficulty concentrating.
- Decreased Blood Flow to the Brain: As blood is diverted to the digestive system, the brain receives less oxygen and nutrients, leading to reduced mental clarity.
- Example: Difficulty focusing on tasks
- Impact: Reduced productivity and mental acuity
- Neurotransmitter Imbalance: Fluctuations in blood sugar levels and hormonal changes can disrupt neurotransmitter balance in the brain, affecting cognitive function.
- Example: Impaired decision-making
- Impact: Decreased mental performance
8.2. Memory and Learning Impairment
Food comas can also impair memory and learning abilities.
- Reduced Hippocampal Activity: The hippocampus, a brain region crucial for memory formation, can be affected by reduced blood flow and glucose availability, impairing memory consolidation.
- Example: Difficulty recalling information
- Impact: Reduced learning efficiency
- Cognitive Fatigue: The mental effort required to process a large meal can lead to cognitive fatigue, making it difficult to retain new information.
- Example: Reduced attention span
- Impact: Impaired memory and learning
8.3. Mood and Emotional Regulation
In addition to affecting cognitive function, food comas can also impact mood and emotional regulation.
- Serotonin Imbalance: The rapid increase in blood sugar levels followed by a crash can disrupt serotonin levels in the brain, leading to mood swings and irritability.
- Example: Increased irritability
- Impact: Mood fluctuations and emotional instability
- Increased Stress Response: The digestive burden associated with a food coma can activate the body’s stress response, leading to feelings of anxiety or unease.
- Example: Feelings of unease
- Impact: Increased stress levels
9. Cultural Perspectives on Food Comas
How do different cultures view the food coma? The experience and perception of food comas can vary across cultures, influenced by dietary habits, social customs, and cultural attitudes towards food and relaxation.
9.1. The American Thanksgiving Tradition
In American culture, the food coma is often associated with Thanksgiving, a holiday characterized by large, elaborate meals and a relaxed atmosphere.
- Cultural Acceptance: The post-Thanksgiving dinner nap is often viewed as a natural and even desirable part of the holiday experience.
- Example: Napping after Thanksgiving dinner
- Impact: Cultural acceptance and expectation
- Overindulgence: Thanksgiving is often a time of overindulgence, with many people consuming far more food than they normally would.
- Example: Large, multi-course meals
- Impact: Increased likelihood of experiencing a food coma
9.2. Mediterranean Cultures and the Siesta
In Mediterranean cultures, the siesta, or afternoon nap, is a traditional practice that may help to mitigate the effects of a food coma.
- Midday Rest: Taking a midday break for rest and relaxation can help to improve digestion and reduce fatigue.
- Example: Siesta in Spain or Italy
- Impact: Improved digestion and reduced fatigue
- Balanced Diet: The Mediterranean diet, which is rich in fruits, vegetables, and healthy fats, may also help to prevent extreme blood sugar fluctuations.
- Example: Emphasis on fresh, whole foods
- Impact: More stable energy levels
9.3. Asian Cultures and Mindful Eating
In some Asian cultures, there is a greater emphasis on mindful eating practices, which may help to prevent overeating and reduce the likelihood of experiencing a food coma.
- Hara Hachi Bu: The Okinawan practice of eating until 80% full can help to prevent overeating and reduce the burden on the digestive system.
- Example: Eating until slightly satisfied
- Impact: Reduced likelihood of overeating
- Focus on Balance: Traditional Asian diets often emphasize balance and moderation, with a focus on whole, unprocessed foods.
- Example: Balanced macronutrient ratios
- Impact: More stable energy levels
10. Research and Studies on Postprandial Somnolence
What does the science say about food comas? Several research studies have explored the physiological mechanisms and potential interventions for postprandial somnolence.
10.1. Studies on Blood Flow and Digestion
Research has shown that after a meal, blood flow is diverted to the digestive system to aid in nutrient absorption. This shift in blood flow can reduce blood supply to other areas of the body, including the brain, leading to feelings of fatigue and reduced mental alertness. According to a study published in the American Journal of Physiology, blood flow to the splanchnic region (the area of the abdomen containing the digestive organs) increases significantly after eating, while blood flow to the brain decreases.
- Findings: Increased blood flow to the digestive system
- Impact: Reduced blood flow to the brain and fatigue
10.2. Hormonal Responses and Insulin
The consumption of food triggers the release of various hormones that play a role in digestion and metabolism. Insulin, in particular, plays a crucial role in regulating blood sugar levels after a meal. A study published in the Journal of Clinical Investigation found that carbohydrate-rich meals can cause a rapid increase in blood sugar levels, prompting the pancreas to release insulin to facilitate glucose uptake by cells. This rapid fluctuation in blood sugar can lead to an initial energy surge followed by a subsequent crash, contributing to the sensation of a food coma.
- Findings: Rapid increase in blood sugar levels and insulin release
- Impact: Energy surge followed by a crash
10.3. Effects of Macronutrient Composition
The macronutrient composition of a meal can also influence the likelihood and severity of postprandial somnolence. A study published in the American Journal of Clinical Nutrition found that meals high in carbohydrates and fats are more likely to induce a food coma compared to meals with a balanced macronutrient profile. Carbohydrates, especially simple sugars, can cause rapid spikes and crashes in blood sugar levels, while fats are more energy-dense and require longer digestion times.
- Findings: High-carbohydrate and high-fat meals are more likely to induce a food coma
- Impact: Energy fluctuations and prolonged digestion
11. Debunking Myths About Food Comas
What are some common misconceptions about food comas? Several myths and misconceptions surround the phenomenon of food comas. Let’s debunk some of the most common ones:
11.1. Myth: It’s Always About the Turkey
Truth: While turkey contains tryptophan, it’s not the sole cause of post-Thanksgiving dinner drowsiness. The large meal size, carbohydrate-rich side dishes, and alcohol consumption also contribute.
11.2. Myth: Food Comas Are Always Bad
Truth: While food comas can be uncomfortable and inconvenient, they are not always a sign of a serious health problem. In most cases, they are a normal physiological response to eating a large meal.
11.3. Myth: You Can Prevent Food Comas Completely
Truth: While you can take steps to minimize the likelihood and severity of food comas, it’s not always possible to prevent them completely, especially when indulging in large, festive meals.
12. Food Coma vs. Other Conditions: What’s The Difference
How is a food coma different from other conditions? It’s important to differentiate a food coma from other conditions that can cause similar symptoms.
12.1. Food Coma vs. Fatigue
Food Coma: Typically occurs after a large meal and is characterized by drowsiness, lethargy, and reduced mental alertness.
Fatigue: Can be caused by a variety of factors, including lack of sleep, stress, and underlying medical conditions.
12.2. Food Coma vs. Hypoglycemia
Food Coma: Often associated with a rapid increase in blood sugar levels followed by a crash.
Hypoglycemia: Characterized by low blood sugar levels, which can cause shakiness, sweating, and confusion.
12.3. Food Coma vs. Narcolepsy
Food Coma: A temporary state of drowsiness that occurs after eating.
Narcolepsy: A chronic neurological disorder characterized by excessive daytime sleepiness and sudden, uncontrollable episodes of falling asleep.
13. Long-Term Effects of Frequent Food Comas
What are the potential long-term effects of frequent food comas? While occasional food comas are generally harmless, frequent occurrences can have long-term health consequences.
13.1. Weight Gain and Obesity
Frequent overeating can lead to weight gain and obesity, increasing the risk of various health problems.
13.2. Metabolic Syndrome
Regularly inducing food comas can contribute to metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and diabetes.
13.3. Digestive Issues
Frequent overeating can strain the digestive system, leading to chronic digestive issues such as bloating, gas, and indigestion.
14. Food Comas and Sleep Quality
How does a food coma affect your sleep? Eating a large meal close to bedtime can interfere with sleep quality and contribute to insomnia.
14.1. Disrupted Sleep Patterns
The digestive process can disrupt sleep patterns, making it difficult to fall asleep and stay asleep.
14.2. Increased Risk of Heartburn
Lying down after eating a large meal can increase the risk of heartburn and acid reflux, which can interfere with sleep.
14.3. Reduced Sleep Efficiency
Eating a large meal before bed can reduce sleep efficiency, leading to less restful and restorative sleep.
15. Addressing Food Comas in the Workplace
How can you manage food comas in a professional setting? Experiencing a food coma at work can be challenging, but there are several strategies you can use to manage the symptoms and maintain productivity.
15.1. Strategies for Staying Alert
- Take a Short Walk: A brief walk can help to improve circulation and boost energy levels.
- Drink Water: Staying hydrated can help to combat fatigue and improve mental alertness.
- Get Some Fresh Air: Spending a few minutes outside can help to refresh your mind and body.
15.2. Dietary Choices at Work
- Pack a Balanced Lunch: Choose a lunch that includes lean protein, whole grains, and plenty of fruits and vegetables.
- Avoid Sugary Snacks: Sugary snacks can lead to energy crashes, so opt for healthier options such as nuts, seeds, or yogurt.
- Practice Portion Control: Avoid overeating by packing smaller portions and eating slowly and mindfully.
15.3. Workplace Accommodations
- Adjust Your Schedule: If possible, schedule your most demanding tasks for times when you’re feeling most alert.
- Take Short Breaks: Regular breaks can help to prevent fatigue and improve concentration.
- Use a Standing Desk: Standing desks can help to improve circulation and boost energy levels.
16. Food Comas and Athletes: A Different Perspective
How do food comas affect athletes? Athletes have unique dietary needs and may experience food comas differently than the general population.
16.1. Fueling for Performance
Athletes need to consume enough calories and nutrients to fuel their training and performance. However, overeating can lead to food comas that can interfere with their athletic performance.
16.2. Timing of Meals
The timing of meals is crucial for athletes. Eating a large meal too close to a workout or competition can lead to digestive discomfort and reduced performance.
16.3. Macronutrient Balance
Athletes need to pay close attention to their macronutrient balance, ensuring that they are consuming enough protein, carbohydrates, and healthy fats to support their training and recovery.
17. The Role of Genetics in Food Comas
Does genetics play a role in how you experience a food coma? Genetic factors can influence metabolism, insulin sensitivity, and other physiological processes that contribute to the likelihood and severity of food comas.
17.1. Metabolic Rate
Genetic variations can affect metabolic rate, influencing how quickly the body processes food and the subsequent impact on energy levels.
17.2. Insulin Sensitivity
Genetic factors can also influence insulin sensitivity, affecting how effectively the body regulates blood sugar levels after a meal.
17.3. Digestive Efficiency
Genetic variations can affect digestive efficiency, influencing how well the body breaks down and absorbs nutrients from food.
18. The Future of Food Coma Research
What’s next for food coma research? Future research may focus on identifying specific genes and biomarkers that contribute to postprandial somnolence, as well as developing personalized dietary and lifestyle interventions to minimize its effects.
18.1. Personalized Nutrition
Personalized nutrition approaches may take into account an individual’s genetic profile, metabolic rate, and other factors to develop tailored dietary recommendations.
18.2. Biomarker Identification
Identifying specific biomarkers that are associated with postprandial somnolence could help to develop diagnostic tests and targeted interventions.
18.3. Lifestyle Interventions
Future research may explore the effectiveness of various lifestyle interventions, such as exercise, stress management, and sleep hygiene, in preventing and managing food comas.
19. Expert Opinions on Food Comas
What do the experts say about food comas? Experts in nutrition, medicine, and physiology offer valuable insights into the phenomenon of food comas.
19.1. Nutritionists
Nutritionists emphasize the importance of portion control, balanced meals, and mindful eating practices in preventing food comas.
19.2. Doctors
Doctors caution against frequent overeating and highlight the potential long-term health consequences of regularly inducing food comas.
19.3. Physiologists
Physiologists study the physiological mechanisms underlying postprandial somnolence, providing a deeper understanding of the hormonal, metabolic, and neurological processes involved.
20. Conclusion: Navigating the Post-Meal Slump
In conclusion, a food coma, or postprandial somnolence, is a common physiological response to eating a large meal, particularly one high in carbohydrates and fats, and FOODS.EDU.VN is dedicated to bringing that knowledge to you. By understanding the causes, symptoms, and potential consequences of food comas, you can make informed dietary and lifestyle choices to minimize their effects and enjoy your meals without the subsequent slump, and also delve deeper into metabolic slowdown and digestive slowdown.
Are you ready to explore more culinary secrets and nutritional insights? Visit FOODS.EDU.VN today! Unlock a world of delicious recipes, expert advice, and in-depth articles that will transform your relationship with food. Our comprehensive resources provide the knowledge you need to make informed choices, optimize your well-being, and elevate your culinary skills. Don’t miss out—join the foods.edu.vn community now and embark on a journey of culinary discovery! Contact us at 1946 Campus Dr, Hyde Park, NY 12538, United States or WhatsApp: +1 845-452-9600.
Frequently Asked Questions (FAQ) about Food Comas
1. What is a food coma?
A food coma, or postprandial somnolence, is the feeling of sleepiness and lethargy that occurs after eating a large meal, particularly one high in carbohydrates and fats.
2. What causes a food coma?
Food comas are caused by physiological changes as the body digests a significant amount of food, including increased blood flow to the digestive system, hormonal responses, and fluctuations in blood sugar levels.
3. Does turkey actually make you sleepy?
While turkey contains tryptophan, an amino acid associated with sleepiness, it’s not the sole cause of post-Thanksgiving dinner drowsiness. The large meal size, carbohydrate-rich side dishes, and alcohol consumption also contribute.
4. What are the symptoms of a food coma?
Common symptoms include sleepiness, lethargy, reduced mental alertness, heaviness, and decreased motivation.
5. How can you prevent a food coma?
You can prevent a food coma by practicing portion control, eating balanced meals, staying hydrated, engaging in light exercise, and limiting alcohol consumption.
6. Are certain medical conditions linked to more intense food comas?
Individuals with diabetes, insulin resistance, digestive disorders, and food allergies or intolerances may experience more pronounced food comas.
7. How does a food coma affect cognitive function?
A food coma can impair cognitive function by reducing alertness and concentration, impairing memory and learning, and affecting mood and emotional regulation.
8. What are some foods that can induce a food coma?
Foods high in carbohydrates, high in fats, and large meals are more likely to induce a food coma.
9. What are some foods that can help prevent a food coma?
Foods high in fiber, lean proteins, and healthy fats can help to prevent a food coma.
10. Are food comas always bad for you?
While food comas can be uncomfortable and inconvenient, they are not always a sign of a serious health problem. In most cases, they are a normal physiological response to eating a large meal.

