Which Food Allergy Increases The Risk Of Latex Allergy? Delve into the fascinating connection between food allergies and latex allergies, uncovering the foods that can trigger cross-reactions and exploring effective management strategies with FOODS.EDU.VN. Discover practical tips for navigating this complex relationship, identify cross-reactive foods, and learn how to minimize exposure to potential allergens, including insights into potential food sensitivities.
1. Understanding the Link Between Latex Allergy and Food Allergies
The connection between latex allergy and certain food allergies is a well-documented phenomenon known as latex-food syndrome or latex-fruit syndrome. This occurs because some proteins found in natural rubber latex are structurally similar to proteins present in various fruits and vegetables. When a person with a latex allergy is exposed to these foods, their immune system may mistakenly identify the food proteins as latex, leading to an allergic reaction.
- Cross-reactivity: The key concept here is cross-reactivity, where the immune system reacts to similar but not identical substances.
- Prevalence: Studies suggest that 30-50% of individuals with latex allergy also experience allergic reactions to certain foods.
- Severity: Reactions can range from mild oral allergy syndrome (itching and tingling in the mouth) to more severe systemic reactions like hives, angioedema (swelling), and even anaphylaxis.
This cross-reactivity highlights the importance of awareness and careful management for individuals with latex allergies. Understanding which foods are most likely to cause problems is crucial for preventing allergic reactions and maintaining a good quality of life. For additional information, FOODS.EDU.VN offers a wealth of resources on food allergies and cross-reactivity.
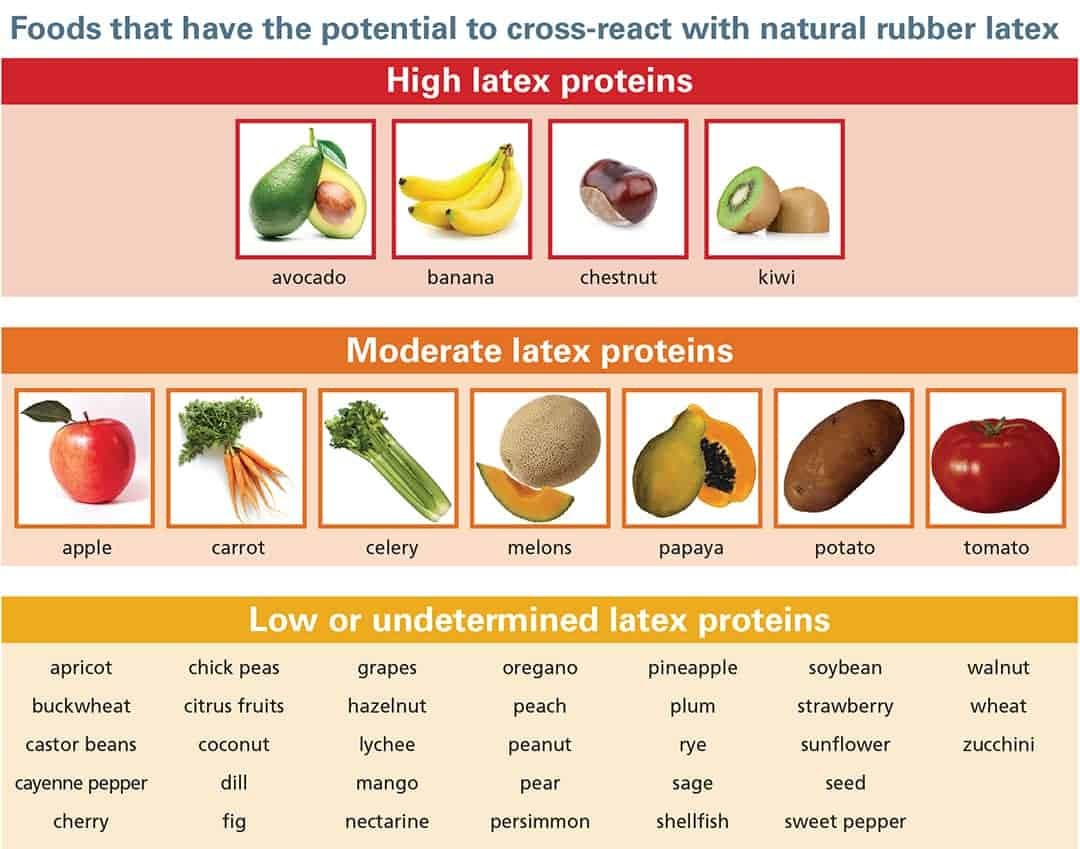
2. The Primary Culprits: Foods with High Cross-Reactivity
While numerous foods have been identified as potential cross-reactors with latex, some stand out as being more commonly associated with allergic reactions in latex-sensitive individuals. These foods share significant protein similarities with latex, making them more likely to trigger a response.
2.1 Avocado
Avocado is a creamy, nutrient-rich fruit that has become increasingly popular. However, it is also one of the most frequently reported cross-reactive foods for people with latex allergies. The protein composition of avocado closely resembles that of latex, increasing the likelihood of an allergic reaction.
- Symptoms: Reactions to avocado in latex-allergic individuals can include oral allergy syndrome, hives, and gastrointestinal distress.
- Prevalence: Studies have shown a significant correlation between avocado allergy and latex allergy.
- Management: Strict avoidance of avocado is often recommended for those with known latex allergy.
 Close-up of a ripe avocado, showcasing its creamy texture and vibrant green color, highlighting its potential as a cross-reactive food allergen for individuals with latex allergies.
Close-up of a ripe avocado, showcasing its creamy texture and vibrant green color, highlighting its potential as a cross-reactive food allergen for individuals with latex allergies.
2.2 Banana
Bananas are a convenient and nutritious snack, but they are also a common cross-reactive food. The proteins in bananas can trigger allergic reactions in latex-sensitive individuals due to their structural similarities to latex proteins.
- Symptoms: Common symptoms include itching, swelling of the mouth and throat, and hives.
- Prevalence: Banana allergy is frequently observed in individuals with latex allergy, particularly children.
- Considerations: Cooking bananas may reduce their allergenicity in some individuals.
2.3 Chestnut
Chestnuts, especially when roasted, are a popular seasonal treat. However, they are also a known cross-reactive food for people with latex allergies. The proteins in chestnuts share similarities with latex proteins, leading to potential allergic reactions.
- Symptoms: Reactions can range from oral allergy syndrome to more severe systemic reactions.
- Prevalence: Chestnut allergy is more common in individuals with latex allergy compared to the general population.
- Recommendations: Avoidance of chestnuts is typically recommended for those with latex allergy.
2.4 Kiwi
Kiwi fruit is a tangy and vitamin-rich fruit that is often used in salads and desserts. However, it is also a high-risk cross-reactive food for individuals with latex allergies. The proteins in kiwi are structurally similar to latex proteins, making it a potential allergen.
- Symptoms: Reactions can include oral allergy syndrome, hives, and even anaphylaxis in severe cases.
- Prevalence: Kiwi allergy is frequently reported in individuals with latex allergy.
- Caution: Due to the risk of severe reactions, strict avoidance of kiwi is often advised.
3. Foods with Moderate and Low Cross-Reactivity
Besides the high-risk foods, several others have been identified as having moderate to low cross-reactivity with latex. While the likelihood of a reaction may be lower, it’s essential to be aware of these foods and monitor for any potential symptoms.
3.1 Moderate Cross-Reactivity Foods
These foods have some degree of protein similarity to latex, but reactions are generally less frequent or less severe compared to the high-risk foods.
- Apple: Apples can cause oral allergy syndrome in some latex-sensitive individuals.
- Carrot: Raw carrots may trigger mild allergic reactions in certain individuals.
- Celery: Celery is a common allergen and can cross-react with latex in some cases.
- Melons: Watermelon, cantaloupe, and honeydew melons have been reported to cause reactions in some individuals with latex allergy.
- Papaya: Papaya contains proteins that may cross-react with latex.
- Potato: Raw potatoes, in particular, may cause allergic reactions.
- Tomato: Tomatoes can cause allergic reactions in some latex-sensitive individuals.
3.2 Low or Undetermined Cross-Reactivity Foods
These foods have a lower likelihood of causing allergic reactions in people with latex allergy. However, it’s still important to be vigilant and monitor for any unusual symptoms.
- Apricot: Apricots are generally considered low-risk for cross-reactivity.
- Buckwheat: Buckwheat is a gluten-free grain that is unlikely to cause reactions.
- Cassava/Manioc: Cassava is a root vegetable that is typically safe for latex-allergic individuals.
- Cherry: Cherries are generally considered low-risk.
- Citrus Fruits: Oranges, lemons, and grapefruits are usually well-tolerated.
- Coconut: Coconuts are not closely related to latex and are typically safe.
- Cucumber: Cucumbers are generally low-risk for cross-reactivity.
- Grape: Grapes are usually well-tolerated.
- Mango: Mangos are considered to have low cross-reactivity.
- Peach: Peaches are generally low-risk.
- Pineapple: Pineapples are typically safe for most latex-allergic individuals.
- Strawberry: Strawberries are generally considered low-risk.
4. Understanding Latex-Fruit Syndrome
Latex-fruit syndrome, also known as latex-food syndrome, is a condition where individuals with latex allergies experience allergic reactions to certain fruits and vegetables due to cross-reactivity. This phenomenon occurs because the proteins in latex are structurally similar to those found in various plant-based foods.
4.1 Causes of Latex-Fruit Syndrome
The primary cause of latex-fruit syndrome is the similarity in protein structures between latex and certain fruits and vegetables. These proteins trigger an immune response in latex-allergic individuals, leading to allergic reactions.
4.2 Symptoms of Latex-Fruit Syndrome
Symptoms of latex-fruit syndrome can vary widely, ranging from mild to severe. Common symptoms include:
- Oral Allergy Syndrome (OAS): Itching, tingling, or swelling of the mouth, lips, tongue, and throat after eating the offending food.
- Hives: Red, itchy bumps on the skin.
- Angioedema: Swelling of the deeper layers of the skin, often affecting the face, lips, and throat.
- Gastrointestinal Symptoms: Nausea, vomiting, abdominal pain, and diarrhea.
- Respiratory Symptoms: Wheezing, coughing, and difficulty breathing.
- Anaphylaxis: A severe, life-threatening allergic reaction that can cause difficulty breathing, dizziness, loss of consciousness, and a drop in blood pressure.
4.3 Management of Latex-Fruit Syndrome
Managing latex-fruit syndrome involves several key strategies:
- Identification of Trigger Foods: Identifying the specific foods that trigger allergic reactions is crucial. This can be done through allergy testing, such as skin prick tests or blood tests (IgE testing).
- Avoidance: Once trigger foods are identified, strict avoidance is necessary to prevent allergic reactions.
- Epinephrine Auto-Injector: Individuals at risk of anaphylaxis should carry an epinephrine auto-injector (EpiPen) and know how to use it.
- Medical Identification: Wearing a medical identification bracelet or necklace can alert healthcare providers to the allergy in case of an emergency.
- Consultation with an Allergist: Regular consultation with an allergist is essential for proper diagnosis, management, and monitoring of the condition.
5. Identifying Your Triggers: Allergy Testing and Elimination Diets
If you have a latex allergy, it’s crucial to identify which foods, if any, are triggering cross-reactions. Several methods can help you pinpoint your specific triggers.
5.1 Allergy Testing
Allergy testing, performed by an allergist, can help determine which foods you are allergic to. Common methods include:
- Skin Prick Test: A small amount of the allergen is placed on the skin, and the skin is pricked to allow the allergen to enter. A raised, itchy bump indicates an allergic reaction.
- Blood Test (IgE Test): A blood sample is tested for the presence of IgE antibodies to specific allergens. Elevated IgE levels indicate an allergic sensitivity.
5.2 Elimination Diet
An elimination diet involves removing suspected trigger foods from your diet for a period of time (usually 2-3 weeks) and then reintroducing them one at a time to monitor for symptoms.
- Process: Work with a healthcare professional or registered dietitian to guide you through the elimination diet.
- Monitoring: Keep a detailed food diary to track your symptoms and identify any potential triggers.
- Reintroduction: Reintroduce foods one at a time, every 2-3 days, and watch for any allergic reactions.
6. Practical Strategies for Managing Latex-Food Syndrome
Living with latex-food syndrome requires careful planning and attention to detail. Here are some practical strategies to help you manage the condition effectively.
6.1 Reading Food Labels
Always read food labels carefully to check for potential allergens. Be aware that ingredients may be listed under different names.
- Hidden Allergens: Watch out for hidden sources of allergens, such as latex gloves used in food preparation.
- Cross-Contamination: Be mindful of cross-contamination in food processing facilities.
6.2 Communicating with Restaurants and Food Service Providers
When eating out, inform the restaurant staff about your latex allergy and any cross-reactive foods you need to avoid.
- Allergen Menus: Ask if they have allergen menus or can provide information about ingredients and preparation methods.
- Safe Preparation: Request that your food be prepared in a separate area to avoid cross-contamination.
6.3 Modifying Recipes
When cooking at home, modify recipes to eliminate any trigger foods.
- Substitutions: Find suitable substitutions for allergenic ingredients.
- Allergy-Friendly Recipes: Explore allergy-friendly recipes and cookbooks.
6.4 Carrying an Epinephrine Auto-Injector
If you are at risk of anaphylaxis, always carry an epinephrine auto-injector (EpiPen) and know how to use it.
- Emergency Plan: Develop an emergency plan with your allergist and share it with family, friends, and caregivers.
- Training: Ensure that those around you know how to recognize the signs of anaphylaxis and administer epinephrine.
6.5 Creating a Safe Home Environment
Minimize exposure to latex and cross-reactive foods in your home.
- Latex-Free Products: Use latex-free gloves, condoms, and other personal care items.
- Safe Food Storage: Store foods properly to prevent cross-contamination.
- Regular Cleaning: Clean surfaces regularly to remove potential allergens.
7. The Role of Cooking and Processing in Reducing Allergenicity
Cooking and processing methods can sometimes reduce the allergenicity of certain foods. Heat can break down proteins, making them less likely to trigger an allergic reaction.
7.1 Cooking
Cooking can alter the protein structure of some foods, reducing their allergenic potential.
- Boiling: Boiling fruits and vegetables may decrease their allergenicity.
- Roasting: Roasting can also denature proteins, making them less allergenic.
- Baking: Baking may reduce the allergenicity of certain foods, such as apples and potatoes.
7.2 Processing
Processing methods like canning, pickling, and fermenting can also modify food proteins and reduce their allergenicity.
- Canning: Canning involves high heat and pressure, which can denature proteins.
- Pickling: Pickling can alter the protein structure of foods.
- Fermenting: Fermentation can break down proteins into smaller, less allergenic components.
However, it’s important to note that cooking and processing may not eliminate the allergenicity of all foods. Some individuals may still react even to cooked or processed foods.
8. Managing Latex Allergy in Children
Children with latex allergy require special attention and care. Parents and caregivers need to be vigilant about avoiding latex exposure and cross-reactive foods.
8.1 Educating Children
Teach children about their allergy and how to avoid potential triggers.
- Age-Appropriate Information: Provide age-appropriate information about latex allergy and cross-reactive foods.
- Empowerment: Empower children to advocate for themselves and communicate their needs to others.
8.2 School and Daycare
Work with school and daycare staff to create a safe environment for your child.
- Allergy Action Plan: Develop an allergy action plan with the school nurse and teachers.
- Emergency Medications: Ensure that emergency medications, such as epinephrine, are readily available and that staff members are trained to administer them.
- Latex-Free Environment: Advocate for a latex-free environment in the classroom and other school areas.
8.3 Food Preparation and Handling
Involve children in food preparation and handling to teach them about safe food practices.
- Reading Labels: Teach children how to read food labels and identify potential allergens.
- Safe Cooking: Supervise children when they are cooking or handling food.
- Handwashing: Emphasize the importance of thorough handwashing to prevent cross-contamination.
9. Recent Research and Emerging Trends in Latex-Food Syndrome
The field of allergy research is constantly evolving, and new studies are shedding light on the complexities of latex-food syndrome.
9.1 Novel Therapies
Researchers are exploring novel therapies for food allergies, including:
- Oral Immunotherapy (OIT): OIT involves gradually increasing the dose of an allergen over time to desensitize the immune system.
- Epicutaneous Immunotherapy (EPIT): EPIT involves applying a patch containing the allergen to the skin.
- Biologic Therapies: Biologic therapies, such as anti-IgE antibodies, can help reduce allergic reactions.
9.2 Diagnostic Advances
New diagnostic tools are being developed to improve the accuracy and efficiency of allergy testing.
- Component-Resolved Diagnostics (CRD): CRD involves testing for IgE antibodies to specific protein components of allergens.
- Basophil Activation Test (BAT): BAT measures the activation of basophils, a type of white blood cell, in response to allergens.
9.3 Prevention Strategies
Researchers are investigating strategies to prevent the development of food allergies in high-risk individuals.
- Early Allergen Introduction: Introducing allergenic foods early in infancy may help prevent the development of allergies.
- Probiotics: Probiotics may help modulate the immune system and reduce the risk of allergies.
10. Expert Opinions and Guidelines
Several organizations and experts provide guidelines and recommendations for managing latex allergy and latex-food syndrome.
10.1 Allergy & Asthma Network
The Allergy & Asthma Network offers resources and support for individuals with allergies and asthma.
- Educational Materials: The organization provides educational materials on latex allergy and cross-reactive foods.
- Support Groups: The Allergy & Asthma Network hosts support groups for individuals with allergies and their families.
10.2 American Academy of Allergy, Asthma & Immunology (AAAAI)
The AAAAI is a professional organization for allergists and immunologists.
- Practice Parameters: The AAAAI publishes practice parameters for the diagnosis and management of allergic diseases.
- Research: The organization supports research on allergies and asthma.
10.3 National Institute of Allergy and Infectious Diseases (NIAID)
NIAID conducts and supports research on allergic diseases.
- Clinical Trials: NIAID sponsors clinical trials to evaluate new therapies for allergies.
- Educational Resources: The institute provides educational resources for healthcare professionals and the public.
11. Case Studies: Real-Life Experiences with Latex-Food Syndrome
Real-life case studies can provide valuable insights into the challenges and successes of managing latex-food syndrome.
11.1 Case Study 1: Sarah’s Story
Sarah, a 32-year-old woman with a known latex allergy, experienced oral allergy syndrome after eating a banana. She underwent allergy testing and was found to be allergic to banana, avocado, and kiwi. Sarah now avoids these foods and carries an epinephrine auto-injector due to the risk of anaphylaxis.
11.2 Case Study 2: Michael’s Experience
Michael, a 10-year-old boy with latex allergy, had a severe allergic reaction after touching a latex balloon at a birthday party. He developed hives, angioedema, and difficulty breathing. Michael’s parents now ensure that his school and daycare are latex-free and that he avoids cross-reactive foods.
11.3 Case Study 3: Emily’s Journey
Emily, a 45-year-old nurse with latex allergy, developed a skin rash after wearing latex gloves at work. She switched to latex-free gloves and avoids cross-reactive foods to minimize her risk of allergic reactions.
12. The Importance of a Multidisciplinary Approach
Managing latex allergy and latex-food syndrome often requires a multidisciplinary approach involving healthcare professionals from various specialties.
12.1 Allergist/Immunologist
An allergist/immunologist can diagnose and manage allergic conditions, including latex allergy and latex-food syndrome.
- Diagnosis: Allergy testing, such as skin prick tests and blood tests.
- Management: Development of an allergy action plan, prescription of emergency medications, and education on allergen avoidance.
12.2 Registered Dietitian
A registered dietitian can provide guidance on dietary modifications and ensure adequate nutrition while avoiding trigger foods.
- Nutritional Assessment: Assessment of nutritional needs and identification of potential deficiencies.
- Meal Planning: Development of meal plans that are both safe and nutritious.
- Recipe Modification: Modification of recipes to eliminate trigger foods.
12.3 Primary Care Physician
A primary care physician can provide ongoing care and coordinate with other healthcare professionals.
- Routine Checkups: Regular checkups to monitor overall health and manage any related conditions.
- Referrals: Referrals to specialists as needed.
12.4 Mental Health Professional
A mental health professional can provide support and guidance for managing the emotional challenges of living with a chronic condition like latex allergy and latex-food syndrome.
- Counseling: Individual or group counseling to address anxiety, depression, or other mental health concerns.
- Coping Strategies: Development of coping strategies for managing the stress of living with a chronic condition.
13. Resources and Support Networks for Latex Allergy Sufferers
Living with latex allergy and latex-food syndrome can be challenging, but numerous resources and support networks are available to help.
13.1 Online Communities
Online communities can provide a sense of connection and support for individuals with latex allergy and their families.
- Forums: Online forums where individuals can share experiences, ask questions, and offer advice.
- Social Media Groups: Social media groups dedicated to latex allergy and food allergies.
13.2 Allergy Organizations
Allergy organizations offer educational resources, support groups, and advocacy efforts.
- Allergy & Asthma Network: Provides educational materials, support groups, and advocacy efforts for individuals with allergies and asthma.
- Food Allergy Research & Education (FARE): Supports research on food allergies and provides educational resources and advocacy efforts.
13.3 Government Agencies
Government agencies offer information and resources on allergies and related conditions.
- National Institute of Allergy and Infectious Diseases (NIAID): Conducts and supports research on allergic diseases and provides educational resources.
- Centers for Disease Control and Prevention (CDC): Provides information on allergies and asthma.
14. Navigating Social Situations with Latex-Food Allergies
Social situations can be particularly challenging for individuals with latex-food allergies. Here are some tips for navigating these situations with confidence:
14.1 Planning Ahead
Plan ahead for social events and communicate your needs to the host.
- Inform the Host: Inform the host about your allergies and any dietary restrictions.
- Offer to Bring a Dish: Offer to bring a dish that you know is safe for you to eat.
- Read Labels: Read labels carefully to ensure that foods are free of allergens.
14.2 Eating Out
When eating out, choose restaurants that are allergy-friendly and communicate your needs to the staff.
- Choose Allergy-Friendly Restaurants: Choose restaurants that are known for accommodating allergies.
- Communicate with Staff: Communicate your allergies to the staff and ask about ingredients and preparation methods.
- Avoid Cross-Contamination: Request that your food be prepared in a separate area to avoid cross-contamination.
14.3 Travel
Traveling with latex-food allergies requires careful planning and preparation.
- Research Destinations: Research destinations to identify allergy-friendly restaurants and accommodations.
- Pack Safe Foods: Pack safe foods and snacks to ensure that you have something to eat if necessary.
- Carry Emergency Medications: Carry emergency medications, such as epinephrine, and ensure that you know how to use them.
15. Long-Term Outlook and Quality of Life
While living with latex allergy and latex-food syndrome can be challenging, with proper management and support, individuals can maintain a good quality of life.
15.1 Management Strategies
Effective management strategies can help minimize the impact of latex allergy and latex-food syndrome on daily life.
- Allergen Avoidance: Strict avoidance of latex and cross-reactive foods.
- Emergency Preparedness: Carrying emergency medications and knowing how to use them.
- Education: Educating yourself and others about latex allergy and latex-food syndrome.
15.2 Support Networks
Support networks can provide emotional support and practical advice for managing latex allergy and latex-food syndrome.
- Online Communities: Online communities where individuals can share experiences and offer advice.
- Allergy Organizations: Allergy organizations that offer educational resources, support groups, and advocacy efforts.
15.3 Emerging Therapies
Emerging therapies, such as oral immunotherapy and biologic therapies, offer hope for improved management of latex allergy and latex-food syndrome.
- Oral Immunotherapy (OIT): Gradually increasing the dose of an allergen over time to desensitize the immune system.
- Biologic Therapies: Biologic therapies, such as anti-IgE antibodies, can help reduce allergic reactions.
FAQ: Frequently Asked Questions About Latex Allergy and Food Cross-Reactivity
-
What is latex-food syndrome? Latex-food syndrome is a condition where individuals with latex allergies experience allergic reactions to certain fruits and vegetables due to cross-reactivity.
-
Which foods are most commonly associated with latex-food syndrome? The most common cross-reactive foods include avocado, banana, chestnut, and kiwi.
-
What are the symptoms of latex-food syndrome? Symptoms can range from mild oral allergy syndrome to severe systemic reactions like hives, angioedema, and anaphylaxis.
-
How is latex-food syndrome diagnosed? Latex-food syndrome is diagnosed through allergy testing, such as skin prick tests or blood tests.
-
How is latex-food syndrome managed? Management involves strict avoidance of trigger foods, carrying an epinephrine auto-injector, and consulting with an allergist.
-
Can cooking reduce the allergenicity of cross-reactive foods? Cooking can sometimes reduce the allergenicity of certain foods, but it may not eliminate the risk of allergic reactions.
-
Are there any emerging therapies for latex-food syndrome? Researchers are exploring novel therapies such as oral immunotherapy and biologic therapies.
-
How can I navigate social situations with latex-food allergies? Plan ahead, communicate your needs to the host, and choose allergy-friendly restaurants.
-
Where can I find support and resources for latex-food allergies? You can find support through online communities, allergy organizations, and government agencies.
-
What is the long-term outlook for individuals with latex-food syndrome? With proper management and support, individuals with latex-food syndrome can maintain a good quality of life.
Understanding the connection between latex allergy and food allergies is crucial for managing this complex condition. By identifying trigger foods, implementing practical strategies, and seeking support from healthcare professionals and support networks, individuals with latex allergy and latex-food syndrome can live full and active lives. For more in-depth information and resources, visit FOODS.EDU.VN, your trusted source for comprehensive food allergy information.
If you’re eager to learn more about food allergies, explore diverse culinary techniques, or find the perfect recipe to suit your dietary needs, FOODS.EDU.VN is your ultimate destination. Don’t miss out—visit FOODS.EDU.VN today and unlock a world of culinary knowledge and inspiration.
Contact us:
Address: 1946 Campus Dr, Hyde Park, NY 12538, United States
Whatsapp: +1 845-452-9600
Website: foods.edu.vn