The epiglottis is the crucial structure that prevents food from entering the trachea, ensuring that food goes down the esophagus and not into your airway, which is vital for breathing and preventing choking; read on with FOODS.EDU.VN to explore the intricate mechanism of the respiratory system and the vital role of the epiglottis, as well as related anatomy, common issues, and preventive measures for maintaining optimal respiratory health, and to explore other areas such as respiratory health tips, pulmonary function, and ENT (ear, nose, and throat) care.
1. What Is The Epiglottis And How Does It Prevent Food From Entering The Trachea?
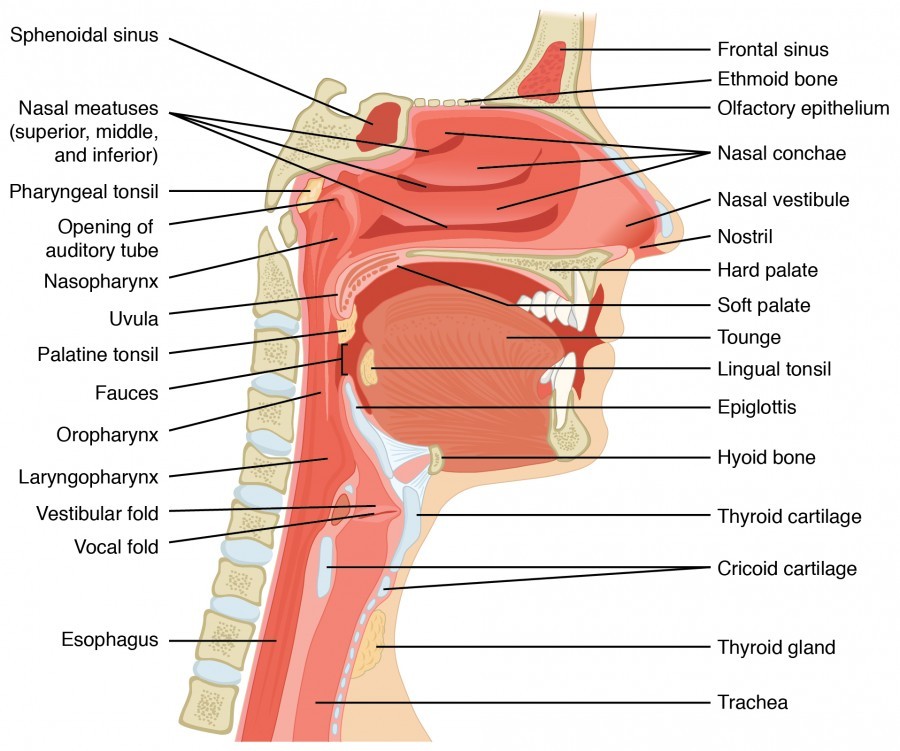
The epiglottis is a leaf-shaped flap of cartilage located in the throat that acts as a crucial gatekeeper, preventing food from entering the trachea and ensuring it goes down the esophagus instead. When you swallow, the epiglottis folds over the entrance of the trachea, creating a secure barrier that directs food and liquids toward the esophagus.
- Anatomical Position: Situated at the base of the tongue, right above the larynx.
- Mechanism of Action: During swallowing, muscles in the throat elevate the larynx, causing the epiglottis to fold down.
- Material Composition: Made of elastic cartilage, allowing flexible movement.
2. What Are The Key Anatomical Structures Involved In Swallowing And Airway Protection?
Several key anatomical structures work together to ensure that swallowing occurs smoothly and that the airway remains protected. These structures include the epiglottis, larynx, pharynx, and associated muscles.
- Larynx (Voice Box): A cartilaginous structure that houses the vocal cords. During swallowing, the larynx moves upward, aiding the epiglottis in sealing off the trachea.
- Pharynx (Throat): A muscular tube that serves as a common pathway for both air and food. It connects the nasal cavity and mouth to the larynx and esophagus.
- Esophagus: A muscular tube that transports food and liquids from the pharynx to the stomach. It lies behind the trachea and shares a close anatomical relationship.
3. How Does The Swallowing Reflex Work And What Role Does The Brain Play?
The swallowing reflex is a complex neurological process coordinated by the brainstem. This reflex ensures that food is safely transported from the mouth to the stomach while protecting the airway.
- Phases of Swallowing:
- Oral Phase: Voluntary movement of food to the back of the mouth.
- Pharyngeal Phase: Involuntary reflex where the soft palate elevates, the epiglottis closes, and the larynx rises.
- Esophageal Phase: Peristaltic waves move food down the esophagus to the stomach.
- Brain’s Role: The medulla oblongata in the brainstem controls the swallowing reflex, coordinating muscle movements and sensory feedback.
4. What Happens If Food Or Liquid Enters The Trachea?
If food or liquid enters the trachea, it can lead to coughing, choking, and potentially serious respiratory complications such as aspiration pneumonia, according to a study by the American Lung Association.
- Immediate Reflexes: The body typically responds with a strong cough reflex to expel the foreign material.
- Aspiration Pneumonia: Occurs when aspirated material causes inflammation and infection in the lungs.
- Choking Hazards: Large pieces of food can obstruct the airway, leading to oxygen deprivation and potentially death if not promptly addressed.
5. What Are Common Disorders That Affect The Epiglottis And Swallowing Function?
Several disorders can affect the epiglottis and swallowing function, leading to difficulties in safely transporting food and liquids. These conditions include epiglottitis, dysphagia, and neurological disorders.
- Epiglottitis:
- Definition: Inflammation of the epiglottis, often caused by bacterial infection.
- Symptoms: Severe sore throat, difficulty swallowing, drooling, and potentially life-threatening airway obstruction.
- Treatment: Immediate medical attention, including antibiotics and potentially intubation to secure the airway.
- Dysphagia:
- Definition: Difficulty swallowing, which can result from various underlying causes.
- Causes: Neurological disorders, structural abnormalities, and age-related changes.
- Symptoms: Coughing or choking while eating, food sticking in the throat, and recurrent pneumonia.
- Management: Speech therapy, dietary modifications, and medical interventions to address the underlying cause.
- Neurological Disorders:
- Conditions: Stroke, Parkinson’s disease, and traumatic brain injury can impair swallowing function.
- Impact: Muscle weakness, incoordination, and sensory deficits can lead to aspiration and malnutrition.
- Rehabilitation: Swallowing therapy and adaptive strategies to improve safety and efficiency of swallowing.
6. How Is Epiglottitis Diagnosed And Treated?
Diagnosing epiglottitis involves a combination of clinical evaluation, imaging studies, and laboratory tests. Prompt diagnosis and treatment are essential to prevent life-threatening airway obstruction, says the Mayo Clinic.
- Diagnostic Methods:
- Clinical Examination: Assessing symptoms such as sore throat, difficulty swallowing, and respiratory distress.
- Laryngoscopy: Visual examination of the larynx and epiglottis using a flexible or rigid scope.
- Neck X-ray: Imaging study to visualize the swelling and inflammation of the epiglottis.
- Blood Cultures: To identify the causative bacterial organism.
- Treatment Strategies:
- Airway Management: Ensuring a patent airway through intubation or tracheostomy if necessary.
- Antibiotics: Intravenous antibiotics to combat bacterial infection.
- Supportive Care: Monitoring vital signs, providing oxygen, and managing pain.
7. What Are The Treatment Options For Dysphagia?
Dysphagia treatment focuses on improving swallowing function and preventing aspiration, which can vary based on the underlying cause and severity of the condition, reports the National Foundation of Swallowing Disorders.
- Speech Therapy:
- Exercises: Strengthening muscles involved in swallowing and improving coordination.
- Compensatory Strategies: Techniques to enhance swallowing safety, such as chin tuck and head rotation.
- Diet Modifications: Altering food textures and consistencies to facilitate easier swallowing.
- Medical Interventions:
- Medications: To manage underlying conditions such as acid reflux or muscle spasms.
- Surgery: In cases of structural abnormalities or tumors affecting swallowing.
- Feeding Tubes: Temporary or permanent feeding tubes for individuals unable to safely swallow food orally.
8. What Are The Long-Term Complications Of Swallowing Disorders?
Swallowing disorders can lead to several long-term complications that impact overall health and quality of life. These complications include malnutrition, dehydration, respiratory infections, and decreased social interaction.
- Malnutrition and Dehydration: Difficulty swallowing can result in inadequate intake of nutrients and fluids, leading to malnutrition and dehydration.
- Respiratory Infections: Aspiration of food and liquids can cause recurrent pneumonia and other respiratory infections.
- Decreased Quality of Life: Swallowing difficulties can affect a person’s ability to enjoy meals, participate in social activities, and maintain independence.
9. How Can You Protect Your Airway While Eating?
Protecting your airway while eating involves adopting safe swallowing practices and modifying dietary habits to minimize the risk of aspiration and choking.
- Tips for Safe Swallowing:
- Sit Upright: Maintain an upright posture while eating to facilitate proper swallowing mechanics.
- Eat Slowly: Take small bites and chew food thoroughly before swallowing.
- Avoid Distractions: Focus on eating and avoid talking or laughing while swallowing.
- Modify Food Consistency: Choose soft, moist foods that are easier to swallow.
- Stay Hydrated: Drink fluids between bites to help moisten food and ease swallowing.
10. What Exercises Can Help Strengthen Swallowing Muscles?
Specific exercises can help strengthen the muscles involved in swallowing, improving overall swallowing function and reducing the risk of aspiration, notes a study in the Journal of Speech, Language, and Hearing Research.
- Exercises to Improve Swallowing:
- Chin Tuck Exercise: Gently tuck your chin towards your chest while swallowing to protect the airway.
- Effortful Swallow: Swallow with increased effort to clear food from the throat.
- Mendelsohn Maneuver: Hold the larynx in an elevated position during swallowing to prolong the opening of the esophagus.
- Tongue Resistance Exercises: Use a tongue depressor to provide resistance while pushing your tongue forward, backward, and sideways.
- Lip Closure Exercises: Practice closing your lips tightly and holding the position to strengthen lip muscles.
11. What Is The Role Of A Speech-Language Pathologist In Managing Swallowing Disorders?
A speech-language pathologist (SLP) plays a crucial role in managing swallowing disorders by assessing swallowing function, developing individualized treatment plans, and providing therapy to improve swallowing safety and efficiency.
- Key Responsibilities of an SLP:
- Swallowing Evaluation: Conducting clinical and instrumental assessments to identify swallowing impairments.
- Treatment Planning: Developing customized therapy programs to address specific swallowing deficits.
- Therapeutic Interventions: Providing exercises, strategies, and dietary recommendations to improve swallowing function.
- Patient Education: Educating patients and caregivers on safe swallowing practices and strategies to prevent complications.
- Collaboration: Working with other healthcare professionals to provide comprehensive care for individuals with swallowing disorders.
12. How Does Aging Affect Swallowing Function?
Aging can affect swallowing function, leading to changes in muscle strength, sensory perception, and overall coordination of the swallowing mechanism. These age-related changes can increase the risk of swallowing difficulties and aspiration, as documented by research from the National Institutes of Health.
- Age-Related Changes in Swallowing:
- Muscle Weakness: Decrease in muscle mass and strength in the tongue, throat, and esophageal muscles.
- Sensory Decline: Reduced sensitivity in the mouth and throat, making it harder to detect food or liquid in the airway.
- Slower Reflexes: Slower swallowing reflexes, which can delay airway protection.
- Increased Risk of Medical Conditions: Higher prevalence of neurological disorders, stroke, and other conditions that affect swallowing function.
- Strategies to Manage Age-Related Swallowing Changes:
- Regular Exercise: Maintain muscle strength and coordination through regular physical activity and targeted swallowing exercises.
- Dietary Modifications: Adjust food textures and consistencies to accommodate changes in swallowing ability.
- Hydration: Ensure adequate fluid intake to prevent dehydration and maintain saliva production.
- Professional Evaluation: Seek evaluation and treatment from a speech-language pathologist if you experience swallowing difficulties.
13. What Are The Latest Advances In The Diagnosis And Treatment Of Swallowing Disorders?
The field of swallowing disorders is continually evolving, with new advances in diagnostic techniques and treatment approaches aimed at improving outcomes for individuals with dysphagia.
- Advances in Diagnosis:
- High-Resolution Manometry: Provides detailed assessment of esophageal pressure and muscle function during swallowing.
- Fiberoptic Endoscopic Evaluation of Swallowing (FEES) with Sensory Testing: Evaluates sensory perception and motor function in the throat during swallowing.
- Video Fluoroscopic Swallowing Study (VFSS) with Dynamic Imaging: Offers real-time visualization of swallowing mechanics and aspiration risk.
- Advances in Treatment:
- Neuromuscular Electrical Stimulation (NMES): Uses electrical stimulation to strengthen and re-educate swallowing muscles.
- Transcranial Magnetic Stimulation (TMS): Non-invasive brain stimulation technique to improve motor control and swallowing function.
- Robotic-Assisted Swallowing Therapy: Utilizes robotic devices to provide precise and targeted exercises for swallowing muscles.
- Drug Therapies: Medications to improve esophageal motility, reduce acid reflux, and manage underlying conditions contributing to dysphagia.
14. How Does The Trachea’s Structure Contribute To Its Function?
The trachea’s structure is uniquely suited to its function of conducting air to and from the lungs, which features C-shaped cartilage rings to provide support while allowing flexibility.
- Structural Components:
- Cartilage Rings: Provide structural support to keep the trachea open and prevent collapse during breathing.
- Fibroelastic Membrane: Connects the open ends of the cartilage rings, allowing the trachea to stretch and recoil during respiration.
- Trachealis Muscle: Smooth muscle located in the fibroelastic membrane that can contract to reduce the trachea’s diameter, increasing the velocity of airflow during coughing.
- Epithelial Lining: Pseudostratified ciliated columnar epithelium with goblet cells that secrete mucus to trap debris and pathogens, and cilia that sweep the mucus upward to be swallowed or expectorated.
- Functional Significance:
- Airway Patency: The cartilage rings ensure that the trachea remains open for efficient airflow.
- Flexibility: The fibroelastic membrane allows the trachea to flex and move with the head and neck.
- Protective Mechanism: The epithelial lining and cilia work together to clear the airway of irritants and infectious agents.
15. What Is The Relationship Between The Esophagus And The Trachea?
The esophagus and trachea are two adjacent structures in the neck that share a close anatomical relationship but serve distinct functions. The esophagus transports food and liquids to the stomach, while the trachea conducts air to and from the lungs.
- Anatomical Proximity: The esophagus lies posterior to the trachea, sharing a common wall in the neck.
- Functional Coordination: During swallowing, the epiglottis closes over the trachea to prevent food from entering the airway, highlighting the coordinated action between these two structures.
- Clinical Significance: Disorders affecting one structure can impact the other. For example, esophageal compression from an enlarged thyroid gland can lead to tracheal narrowing and breathing difficulties.
16. How Do Vocal Cords Contribute To Airway Protection?
Vocal cords, or true vocal folds, play a crucial role in airway protection by providing a tight seal to prevent aspiration of food and liquids into the trachea.
- Protective Mechanisms:
- Adduction: The vocal cords adduct (close) during swallowing to prevent aspiration.
- Cough Reflex: Sensory receptors in the larynx trigger a cough reflex if foreign material enters the airway.
- Laryngeal Closure Reflex: The larynx quickly closes to protect the airway from irritants and pathogens.
- Clinical Implications:
- Vocal Cord Paralysis: Can impair airway protection and increase the risk of aspiration.
- Laryngospasm: Sudden, involuntary contraction of the vocal cords can cause airway obstruction.
17. What Are The Symptoms Of Aspiration?
Aspiration occurs when food, liquid, or other foreign material enters the airway and lungs, leading to various symptoms that can range from mild to severe, per the American Thoracic Society.
- Common Symptoms of Aspiration:
- Coughing or Choking: During or immediately after eating or drinking.
- Wet or Gurgly Voice: After swallowing.
- Shortness of Breath or Wheezing: Indicating airway obstruction or inflammation.
- Chest Discomfort or Pain: Suggesting lung irritation or infection.
- Recurrent Pneumonia: Repeated lung infections due to chronic aspiration.
- Fever: A sign of infection in the lungs.
- Increased Congestion or Mucus Production: In the airways.
- Unexplained Weight Loss: Due to difficulty eating and absorbing nutrients.
18. How Is Aspiration Diagnosed?
Diagnosing aspiration involves a combination of clinical assessment, imaging studies, and swallowing evaluations to determine if food or liquid is entering the airway and lungs.
- Diagnostic Tests for Aspiration:
- Clinical Swallowing Evaluation: Assessment of oral motor skills, swallowing mechanics, and signs of aspiration during eating and drinking.
- Modified Barium Swallow Study (MBSS): Real-time X-ray imaging of swallowing to visualize aspiration and identify swallowing abnormalities.
- Fiberoptic Endoscopic Evaluation of Swallowing (FEES): Visual examination of the throat and larynx using a flexible endoscope to assess swallowing function and aspiration risk.
- Chest X-ray: Imaging study to detect signs of pneumonia or lung damage resulting from aspiration.
- Sputum Culture: Laboratory analysis of sputum to identify bacteria or other pathogens in the lungs.
19. What Are The Treatment Options For Aspiration?
Treatment options for aspiration focus on improving swallowing safety, preventing lung damage, and managing any complications that may arise.
- Treatment Approaches for Aspiration:
- Swallowing Therapy: Exercises and strategies to improve swallowing muscle strength, coordination, and airway protection.
- Diet Modifications: Changing food textures and consistencies to make swallowing easier and safer.
- Postural Techniques: Adjusting body position during eating to reduce aspiration risk, such as chin tuck or head rotation.
- Medications: To manage underlying conditions such as acid reflux or infections.
- Feeding Tubes: Temporary or permanent feeding tubes to provide nutrition if oral intake is unsafe.
- Pulmonary Hygiene: Techniques to clear the airways of secretions and prevent pneumonia, such as coughing, deep breathing exercises, and chest physiotherapy.
20. What Lifestyle Modifications Can Reduce The Risk Of Aspiration?
Adopting certain lifestyle modifications can significantly reduce the risk of aspiration, particularly for individuals with swallowing difficulties or other risk factors.
- Lifestyle Changes to Prevent Aspiration:
- Eat Slowly and Mindfully: Take small bites, chew food thoroughly, and avoid distractions while eating.
- Sit Upright While Eating: Maintain an upright posture during meals and for at least 30 minutes afterward.
- Avoid Talking While Eating: Focus on swallowing and avoid conversations that can interfere with coordination.
- Stay Hydrated: Drink fluids regularly to keep the throat moist and aid swallowing.
- Limit Alcohol and Sedatives: These substances can impair swallowing reflexes and increase aspiration risk.
- Quit Smoking: Smoking can damage the airways and impair the cough reflex, increasing susceptibility to aspiration.
- Maintain Good Oral Hygiene: Regular brushing and flossing can reduce the risk of bacterial infections in the mouth and throat.
21. What Is The Role Of Mucus In Protecting The Respiratory System?
Mucus plays a vital role in protecting the respiratory system by trapping pathogens, irritants, and debris, which are then cleared from the airways by the mucociliary escalator.
- Protective Functions of Mucus:
- Trapping Pathogens: Mucus contains antibodies and antimicrobial substances that neutralize bacteria, viruses, and fungi.
- Filtering Irritants: Mucus traps dust, pollen, smoke, and other airborne particles, preventing them from reaching the lungs.
- Hydrating Airways: Mucus helps keep the airways moist, preventing dryness and irritation.
- Facilitating Clearance: The mucociliary escalator, composed of cilia and mucus, sweeps trapped debris upward to be swallowed or expectorated.
- Factors Affecting Mucus Production:
- Infections: Respiratory infections can increase mucus production, leading to congestion and cough.
- Allergies: Allergic reactions can cause inflammation and increased mucus secretion in the airways.
- Dehydration: Inadequate fluid intake can result in thicker, stickier mucus that is harder to clear.
- Smoking: Smoking can damage the cilia and impair the mucociliary escalator, leading to mucus buildup.
22. How Does Coughing Help Clear The Airway?
Coughing is a powerful reflex mechanism that helps clear the airway of irritants, secretions, and foreign material, preventing them from reaching the lungs.
- Mechanism of Coughing:
- Irritant Detection: Sensory receptors in the airways detect irritants or excess mucus.
- Inspiratory Phase: Deep breath taken to increase lung volume.
- Compressive Phase: Glottis closes, and chest muscles contract to build up pressure in the lungs.
- Expulsive Phase: Glottis suddenly opens, and air is forcefully expelled, carrying with it any irritants or secretions.
- Effectiveness of Coughing:
- Clearing Airways: Coughing can remove mucus, debris, and foreign objects from the trachea and bronchi.
- Preventing Infections: By clearing the airways, coughing helps prevent the buildup of pathogens that can lead to pneumonia and other respiratory infections.
- Types of Cough:
- Voluntary Cough: Initiated consciously to clear the airway.
- Involuntary Cough: Triggered by irritants or inflammation in the respiratory tract.
- Productive Cough: Produces mucus or phlegm.
- Non-Productive Cough: Dry cough that does not produce mucus.
23. What Is The Heimlich Maneuver And When Should It Be Used?
The Heimlich maneuver is a life-saving technique used to dislodge an object obstructing a person’s airway, preventing choking and potential death, explains the American Red Cross.
- How to Perform the Heimlich Maneuver:
- Assess the Situation: Determine if the person is choking and unable to breathe, cough, or speak.
- Stand Behind the Person: Wrap your arms around their waist.
- Make a Fist: Place the thumb side of your fist against the middle of their abdomen, slightly above the navel.
- Grasp Your Fist: With your other hand and give quick, upward thrusts into their abdomen.
- Repeat: Continue thrusts until the object is dislodged, or the person becomes unconscious.
- When to Use the Heimlich Maneuver:
- Choking: When a person is unable to breathe, cough, or speak due to an obstructed airway.
- Universal Choking Sign: If the person is clutching their throat with their hands.
- Modifications:
- For Pregnant Women or Obese Individuals: Perform chest thrusts instead of abdominal thrusts, placing your hands on the lower half of the breastbone.
- For Infants: Use back blows and chest thrusts while holding the infant face down over your forearm.
24. How Does Smoking Affect The Epiglottis And Airway?
Smoking has detrimental effects on the epiglottis and airway, increasing the risk of inflammation, infection, and impaired function, reports the Centers for Disease Control and Prevention.
- Harmful Effects of Smoking:
- Inflammation: Smoking irritates and inflames the lining of the airway, leading to chronic bronchitis and other respiratory conditions.
- Cilia Damage: Smoking damages the cilia, impairing their ability to clear mucus and debris from the airways.
- Increased Mucus Production: Smoking stimulates the production of excess mucus, which can clog the airways and increase the risk of infection.
- Impaired Immune Function: Smoking weakens the immune system, making the airways more susceptible to infections.
- Increased Cancer Risk: Smoking increases the risk of cancers of the larynx, trachea, and lungs.
25. What Are The Benefits Of Staying Hydrated For Respiratory Health?
Staying hydrated is essential for maintaining optimal respiratory health by keeping the airways moist, thinning mucus, and supporting immune function, clarifies the American Lung Association.
- Benefits of Hydration:
- Moistening Airways: Adequate fluid intake helps keep the airways moist, preventing dryness and irritation.
- Thinning Mucus: Hydration thins mucus, making it easier to clear from the airways and reducing congestion.
- Supporting Immune Function: Proper hydration supports the immune system, helping the body fight off respiratory infections.
- Preventing Dehydration: Dehydration can thicken mucus and impair the function of the mucociliary escalator, increasing the risk of respiratory complications.
26. How Can Allergies Affect The Respiratory System?
Allergies can significantly affect the respiratory system, leading to inflammation, increased mucus production, and airway constriction, which can cause symptoms such as sneezing, coughing, and difficulty breathing, notes the Asthma and Allergy Foundation of America.
- Impact of Allergies on the Respiratory System:
- Inflammation: Allergic reactions trigger inflammation in the airways, causing swelling and irritation.
- Increased Mucus Production: Allergies can stimulate the production of excess mucus, leading to congestion and cough.
- Airway Constriction: Allergic reactions can cause the muscles around the airways to tighten, making it harder to breathe.
- Asthma Symptoms: Allergies can worsen asthma symptoms, leading to wheezing, shortness of breath, and chest tightness.
- Managing Allergies:
- Avoidance: Identify and avoid allergens that trigger respiratory symptoms.
- Medications: Antihistamines, decongestants, and corticosteroids can help relieve allergy symptoms.
- Immunotherapy: Allergy shots can desensitize the immune system to specific allergens, reducing the severity of allergic reactions.
27. What Is The Importance Of Proper Posture For Breathing And Swallowing?
Proper posture is crucial for optimizing breathing and swallowing by ensuring that the airways are open, the muscles are aligned, and the swallowing mechanism functions efficiently.
- Benefits of Good Posture:
- Open Airways: Maintaining an upright posture helps keep the airways open, allowing for efficient airflow.
- Muscle Alignment: Good posture aligns the muscles of the neck and throat, optimizing their function during swallowing.
- Efficient Swallowing: Proper posture supports the coordination of the swallowing mechanism, reducing the risk of aspiration.
- Reduced Strain: Good posture reduces strain on the neck and throat muscles, preventing fatigue and discomfort.
- Tips for Maintaining Good Posture:
- Sit Upright: Sit with your back straight, shoulders relaxed, and feet flat on the floor.
- Avoid Slouching: Be mindful of your posture throughout the day and avoid slouching or hunching over.
- Use Proper Support: Use supportive chairs and pillows to maintain good posture while sitting and sleeping.
- Take Breaks: Take frequent breaks to stretch and move around, preventing muscle stiffness and fatigue.
28. How Does Exercise Benefit Respiratory Health?
Regular exercise offers numerous benefits for respiratory health, including improving lung function, strengthening respiratory muscles, and enhancing overall endurance, confirms research from the American College of Sports Medicine.
- Benefits of Exercise for Respiratory Health:
- Improved Lung Function: Exercise increases lung capacity and efficiency, allowing for better oxygen uptake and carbon dioxide removal.
- Strengthened Respiratory Muscles: Regular physical activity strengthens the muscles involved in breathing, making it easier to breathe deeply and efficiently.
- Enhanced Endurance: Exercise increases overall endurance, reducing shortness of breath and fatigue during physical activity.
- Reduced Risk of Respiratory Diseases: Regular exercise can lower the risk of developing chronic respiratory diseases such as asthma and COPD.
- Types of Exercise:
- Aerobic Exercise: Activities such as walking, running, swimming, and cycling improve cardiovascular and respiratory function.
- Strength Training: Exercises that strengthen the muscles of the chest, back, and abdomen can improve breathing mechanics.
- Breathing Exercises: Techniques such as diaphragmatic breathing and pursed-lip breathing can improve lung capacity and efficiency.
29. What Are Some Common Misconceptions About Swallowing And Airway Protection?
Several misconceptions exist regarding swallowing and airway protection, leading to confusion and potentially harmful practices, which is why it’s essential to understand these myths and disseminate evidence-based information.
- Common Misconceptions:
- Myth: You can’t aspirate if you’re not coughing.
- Fact: Silent aspiration can occur without triggering a cough reflex, making it difficult to detect.
- Myth: Drinking thin liquids is always safe for people with swallowing difficulties.
- Fact: Thin liquids can be challenging to control and may increase the risk of aspiration for some individuals.
- Myth: Swallowing problems are a normal part of aging.
- Fact: While age-related changes can affect swallowing, significant swallowing difficulties should be evaluated and treated.
- Myth: Feeding tubes are a last resort for people with swallowing disorders.
- Fact: Feeding tubes can be a valuable tool for providing nutrition and preventing malnutrition in individuals who cannot safely swallow food orally.
- Myth: You can’t aspirate if you’re not coughing.
30. Where Can I Find More Information And Support For Swallowing Disorders?
Numerous resources are available to provide information, support, and guidance for individuals with swallowing disorders and their caregivers.
- Resources for Swallowing Disorders:
- FOODS.EDU.VN: Offers comprehensive articles, practical advice, and the latest research to improve respiratory health, and provides detailed guidance and practical tips to manage and protect your respiratory system.
- The American Speech-Language-Hearing Association (ASHA): Provides information on swallowing disorders, speech therapy, and finding qualified professionals.
- The National Foundation of Swallowing Disorders (NFOSD): Offers resources, support groups, and educational materials for individuals with dysphagia.
- The American Lung Association: Provides information on respiratory health, lung diseases, and smoking cessation.
- Medical Professionals: Consult with doctors, speech-language pathologists, and other healthcare providers for personalized advice and treatment options.
Understanding the epiglottis and its role in preventing food from entering the trachea is essential for maintaining respiratory health and preventing complications. By adopting safe swallowing practices, seeking professional help when needed, and staying informed about the latest advances in diagnosis and treatment, individuals can effectively manage swallowing disorders and protect their airways. Remember, FOODS.EDU.VN is always here to provide you with the knowledge and support you need to live a healthier, more informed life.
Want to learn more about how to maintain a healthy respiratory system and explore a wealth of information on nutrition, food science, and healthy eating habits? Visit foods.edu.vn at 1946 Campus Dr, Hyde Park, NY 12538, United States, or contact us via WhatsApp at +1 845-452-9600, and dive into our expertly crafted articles, practical tips, and the latest research to empower your journey towards better health.
FAQ: Structures Preventing Food From Entering The Trachea
- What is the primary function of the epiglottis?
The primary function of the epiglottis is to prevent food and liquids from entering the trachea (windpipe) during swallowing, ensuring that they pass safely into the esophagus. - Where is the epiglottis located in the human body?
The epiglottis is located in the throat, just behind the tongue and above the larynx (voice box). It is attached to the entrance of the larynx. - How does the epiglottis work during the swallowing process?
During swallowing, the epiglottis folds downward to cover the opening of the larynx, creating a barrier that directs food and liquids toward the esophagus instead of the trachea. - What other structures help protect the airway during swallowing?
Besides the epiglottis, the vocal cords and the elevation of the larynx also help protect the airway during swallowing. - What happens if the epiglottis doesn’t function properly?
If the epiglottis doesn’t function properly, food or liquids can enter the trachea, leading to coughing, choking, and potentially aspiration pneumonia. - What is aspiration pneumonia?
Aspiration pneumonia is a type of lung infection that occurs when food, saliva, liquids, or vomit is inhaled into the lungs instead of being swallowed into the esophagus. - What are some common symptoms of aspiration?
Common symptoms of aspiration include coughing during or after eating, a wet or gurgly voice after swallowing, shortness of breath, and chest discomfort. - How can aspiration be diagnosed?
Aspiration can be diagnosed through clinical swallowing evaluations, modified barium swallow studies (MBSS), and fiberoptic endoscopic evaluations of swallowing (FEES). - What are some strategies to protect the airway while eating?
Strategies to protect the airway while eating include sitting upright, eating slowly, taking small bites, chewing food thoroughly, and avoiding distractions. - When should someone seek medical attention for swallowing difficulties?
Someone should seek medical attention for swallowing difficulties if they experience frequent coughing or choking while eating, food sticking in their throat, recurrent pneumonia, or unexplained weight loss.